Key Points
- Myth: CKD is rare (a mild form is quite common)
- Myth: CKD makes you feel unwell (it’s a silent disease in its early stages)
- Myth: CKD leads to dialysis (that is rare)
- Myth: Drinking a lot of water is ‘good’ for the kidneys (it is not)
- Myth: Kidney problems cause back pain (also rare)
Chronic Kidney Disease (CKD) means a long term impairment of kidney function. We will now describe 10 CKD myths.
1. Myth: Chronic kidney disease is a rare condition
Fact. You may be surprised to learn just how common kidney disease is. A mild form is common, affecting 10% of the population. What puts you at risk? Having high blood pressure, diabetes, a family history of kidney failure, and being over 60 years are the major risk factors for kidney disease.
Fortunately, severe kidney disease (CKD5 or kidney failure, see below) is rare. In fact, every GP will have only one patient on dialysis or with a transplant on their books.
2. Myth: You’ll be able to tell if you have kidney disease
Fact. Unfortunately, most people who have kidney disease don’t know it. Why not? Because in the early stages of CKD (called CKD1 to CKD3, see below), most people do not have any symptoms. It is a ‘silent disease’, like diabetes (in its early stages) and high blood pressure. Symptoms may not appear until CKD is in the advanced stages (called CKD4 or CKD5, see below). The best way to find out if you have kidney disease is to get tested – and once you are diagnosed, there are many steps you can take to reduce the progression of the disease.
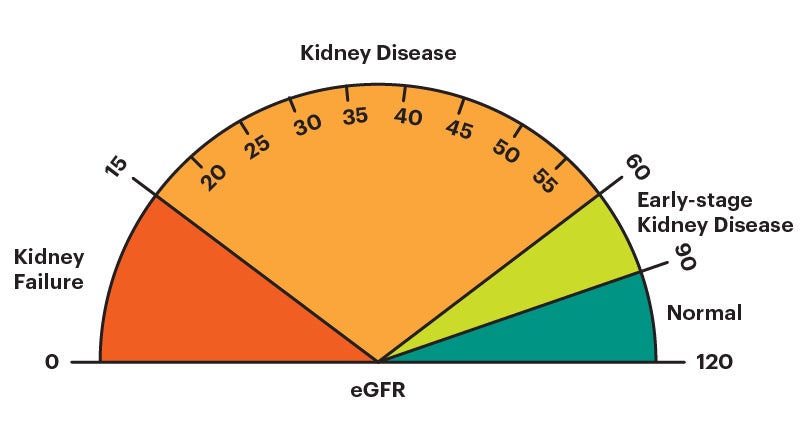
There is a classification of severity of CKD based on something called eGFR. Normal eGFR in humans is 90-120 mls/min. The CKD classification has 5 grades:
CKD1+2: risk factors for CKD (eGFR 60-120 mls/min) – no symptoms
CKD3: mild CKD (eGFR 30-59 mls/min) – no or very mild symptoms
CKD4: moderate CKD (eGFR 15-29 mls/min) – moderate symptoms
CKD5: severe CKD (kidney failure; eGFR < 15 mls/min) – severe symptoms (require dialysis or a transplant).
3. Myth: CKD is curable
Fact. Chronic kidney disease is not curable. However, progression of the disease to kidney failure can be slowed, especially if it is detected early. Kidney failure is not inevitable. In fact, few patients with CKD get kidney failure (CKD5).
However, if CKD progresses to kidney failure, either dialysis or kidney transplant will be necessary.
4. Myth: A kidney transplant will cure CKD
Fact. Along with the previous point, some may have the misconception that a kidney transplant is a cure for chronic kidney disease. Just like the disease can be slowed, but not completely cured (through medication or lifestyle changes), a kidney transplant is another treatment that can aid in your overall condition but cannot cure it completely.
A well functioning transplant will provide 45-60 ml/min of GFR, i.e. half of normal human GFR; and the blood creatinine will be normal (under 120 mcmol/L).
The average kidney transplant (from a deceased donor) has a lifespan of about 10 years – or 15 years if it’s from a living donor. Regardless of which donor is used, patients will need to continue taking immunosuppressive medication (to prevent rejection) for the remainder of their life.
5. Myth: Drinking a lot of water is ‘good’ for the kidneys (especially in CKD)
Fact. Drinking lots of water might seem like a good idea, and of course it is important to get enough fluid into your body. But it does not ‘flush out the kidneys’. And for many patients with CKD, too much fluid intake can actually cause ‘oedema’ (swelling, especially around the ankles), as well as high blood pressure and breathing problems. So many patients, in fact, are asked to restrict their fluids to say 2 litres, 1.5L or even 1L per day.
If you have CKD, you should talk to your doctor, nurse or dietitian about the correct, healthy fluid intake for you.
6. Myth: Testing for CKD is a long and complicated process
Fact. Testing for kidney disease is surprisingly easy. It can be done with two simple, inexpensive tests during a routine visit with your doctor.
- A simple blood test called creatinine (normal range 60-120 mcmol/L), which leads to an estimated GFR (or ‘eGFR’; glomerular filtration rate). This is normally 90-120 mls/min. These numbers tell you how well your kidneys are working – the lower the creatinine, and higher the eGFR, the better.
- A simple urine test to check for protein (called ACR) in your urine. Having a raised level of protein in your urine can be a sign kidney disease. All humans have a small amount of it.
7. Myth: No one knows what causes kidney disease
Fact. It is true that of all the people on dialysis or with a transplant, the commonest ’cause’ is uncertain (30%). But we do know a lot about the other 70%. Of them, the biggest known cause is diabetes (20%). After that the biggest groups of causes are:
- Renovascular disease = blockage to the arteries (blood vessels) to the kidneys. Both have to be blocked or half blocked
- Glomerulonephritis = a group of ‘autoimmune’ conditions where the body’s immune system (defender) attacks the glomeruli, which are the tiny filters in the kidney (a million in each)
- Tubulointerstitial disease = damage to the tiny tubes that drain urine from the glomeruli
- Obstruction to the urinary tract = blockage to the bladder, or kidneys, or ureters (the tubes that connect them) – or prostate in a man. If the cause is the kidneys or ureters, again both have to be blocked or half blocked
- Polycystic kidney disease = the only common inherited cause.
8. Myth. I have back pain so it must be my kidneys
Fact. Kidney disease rarely causes back pain. Pain in the back may occasionally come from kidney disease if you have infection or blockage in one or both kidneys. Other forms of kidney disease rarely cause pain in the back.
 Site of kidney pain – a rare cause of back pain
Site of kidney pain – a rare cause of back pain
The most common cause of back pain is disease of the spine or back muscles, and not kidney disease. The kidney can only feel pain if the covering of the kidney (called the capsule) is stretched. This means swelling of the kidney from either infection or blockage of urine flow (such as due to a kidney stone) can result in pain. Typically kidney pain spreads from the side of the back (under the ribs), and may come around the side to cause pain down into the groin area.
Patients with CKD often also state “I don’t have any trouble passing my urine so my kidneys must be fine”. Also, not true. Even patients who are on dialysis make urine. Damaged kidneys will continue to make urine, even if they no longer properly clean your blood.
9. Myth: Kidney stones cause CKD
Fact. While kidney stones are not pleasant, they do not usually lead to kidney disease. Cases of kidney stones resulting in permanent damage to the kidneys are very rare.
High blood pressure is also a rare cause of CKD, though most patients with CKD have high blood pressure – so the two are linked. There is more about high blood pressure on myHSN.
10. Myth: If you are at risk for kidney disease, there is nothing you can do about it
Fact. Many people have the misconception that kidney disease is caused by genetics and therefore not preventable. However, in many cases, kidney disease is preventable (to an extent) – or, if not preventable, at least partially treatable
One of the most important things you can do, is to have the diagnosis made as soon as possible (at the CKD3 stage or earlier). Then, if your GP thinks it necessary, you should see a kidney specialist (called a nephrologist or renal physician) at the hospital soon afterwards.
Other things you can do include: controlling your blood pressure, reducing the amount of salt and protein in your diet (if requested), stopping smoking, losing weight (if you need to) and exercising regularly.
Summary
We have described 10 CKD myths. We hope you have found it helpful.
Last Reviewed on 4 April 2024
