10 CKD quick facts – chronic kidney disease
Keep track of your kidney data with PKB
Key points
- Where are the kidneys? Near the middle of your lower back, on either side of spine
- What do the kidneys do? Body’s dustmen
- What is CKD (chronic kidney disease)? – long term reduction in kidney function (or abnormal kidney structure). A mild form is very common – affecting up to 10% of the population. Only 1 in 100 people end up requiring dialysis or a kidney transplant. Average age group for starting dialysis is 60-65 years
- How is CKD diagnosed? CKD stage/eGFR classification
- Causes of CKD – 7 groups – unknown (with small kidneys) and diabetes are the commonest
- Symptoms of CKD – shortness of breath and ankle swelling are red flag symptoms
- What treatment can the doctor offer? Even though CKD is not normally curable, there is alot doctors and the NHS can do. Does everyone with CKD need treatment? No
- What can I do to help myself? There are THREE important things you should do: know your numbers (eGFR/creatinine), keep BP low (130/80 or less all the time), lose weight (if overweight)
- How often do I need my eGFR/creatinine measured? – very variable
- What is the outlook for CKD? – generally good, but very variable.
1. Where are the kidneys? Near the middle of your lower back, on either side of spine
They are higher up than most people think. The kidneys are protected from injury by a large layer of fat, along with your lower ribs and back muscles.
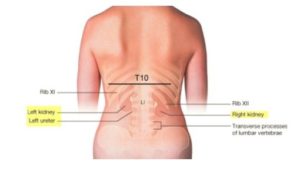
They are about the size of your palm: 12cm long, 6cm wide and 3cm deep. Each kidney weighs about 150g.
2. What do the kidneys do? Body’s dustmen
The normal function of the kidneys is to be the body’s dustmen and keep the levels of chemicals and water stable in the blood.
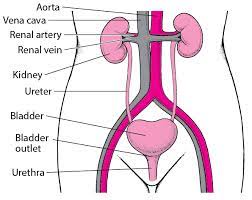
To do this, the kidneys receive approximately 20-25% of the blood from the heart. This blood from the heart enters the kidneys through the renal artery (see above) and goes back into your body by the renal vein. The kidney filters the blood to remove waste products and extra water.
The kidneys pass the filtered blood into the urine that emerges from the urethra when you wee.
3. What is CKD (chronic kidney disease)? – long term reduction in kidney function (or abnormal structure)
CKD can also be a problem with the structure of the kidneys (with normal function). It affects both kidneys, and usually comes on over months or years.
A mild form is very common – affecting up to 10% of the population. Only 1 in 100 people end up requiring dialysis or a kidney transplant
CKD may result in failure to maintain the balance of water and chemicals (including acid) in the body.
Risk factors = age, male gender, being Black and Asian, smoking, family history, and previous acute kidney injury (AKI) episode(s).
4. How is CKD diagnosed? CKD/eGFR classification
It is surprisingly easy to diagnose, define and classify. It requires more than a doctor taking a history (asking questions) and examining you – but that should happen as well. After that, you will need these 3 big tests:
- Blood tests – mainly eGFR and creatinine (on which GFR is based) – higher the GFR, lower the creatinine the better
- Urine tests – mainly the protein level (as indicated by the urine ACR, uACR) – the lower the uACR the better
- Kidney ultrasound scan (in many). It should show two normal kidneys >10cm in length.
After that, CKD is classified according to its severity, based on the called eGFR (estimated glomerular filtration rate) – the higher the eGFR, the better the function. Normal eGFR in humans is 90-120 mls/min. The eGFR is based on a simple blood test called creatinine (normal range 60-120 mcmol/L); the lower the creatinine, the higher is the GFR, the better.
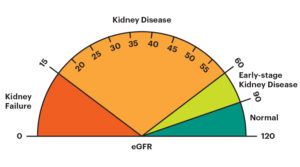
The CKD classification has 5 grades. See the diagram above.
- CKD1+2 – risk factors for CKD (eGFR 60-120 mls/min)
- CKD3A – mild CKD (eGFR 45-59 mls/min)
- CKD3B – mild CKD (eGFR 30-44 mls/min)
- CKD4 – moderate CKD (eGFR 15-29 mls/min)
- CKD5 – severe CKD (kidney failure) (eGFR < 15 mls/min)
– CKD4 means you may require dialysis or a kidney transplant one day.
– CKD5 means you require dialysis, or a kidney transplant, or supportive care (no dialysis).
5. Causes of CKD – 7 groups – unknown (with small kidneys) and diabetes are the commonest
- Unknown (often with small kidneys). This is the ‘cause’ in 30% of patients
- Diabetes (mainly type 2). This is the cause in 20% of patients, i.e. the second commonest
- Renovascular disease. This mainly occurs in older people who are smokers or ex-smokers; and/or people with congestive heart failure. It is then called ‘cardiorenal syndrome’
- Obstructive nephropathy. This means a blockage in the drainage system of the kidneys – i.e. ureters, bladder, or prostate (in men). It is usually due to prostatic disease in a men, or cancer in the pelvis in women. Kidney stones can cause it, but are not a common cause (unless you have one kidney)
- Glomerulonephritis / vasculitis. These are ‘autoimmune’ (of which there are 7 types). This means the body’s immune system (normally its defender) attacks the glomeruli (tiny filters within the kidneys)
- Tubulointerstitial disease (TID). ‘Tubulointerstitial disease’ is not really just one diagnosis. There are three groups of causes of TID including: autoimmune, drugs and infection (e.g. reflux nephropathy). The drug causes include non-steroidal anti-inflammatory drugs (NSAIDs; if they are used long-term, especially at high doses), lithium, ciclosporin and tacrolimus
- Polycystic kidney disease. This is an inherited condition where multiple cysts form on the kidney. It is the only common familial (inherited) cause.
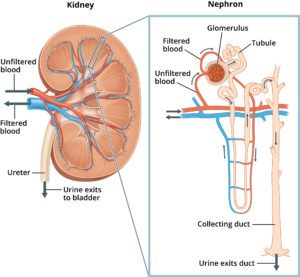
Glomeruli and tubules of the kidneys.
Notes. Simple primary (essential) high blood pressure and simple recurrent urinary tract infections (UTIs) do not cause CKD. A doctor should find another cause in such a patient with simple high BP or UTIs.
6. Symptoms of CKD – shortness of breath and ankle swelling are red flag symptoms
- Tiredness
- Weight loss (or gain) and poor appetite
- Itching and pain
- Difficulty sleeping (insomnia) and concentrating
- Frothy urine and an increased need to pee – particularly at night
- Swollen ankles, feet, hands or face (especially around the eyes) – as a result of water retention (oedema). This is a red flag symptom
- Shortness of breath – also a result of water retention. Shortness of breath is also a red flag symptom in CKD, and should never be ignored.
Note. There may be no symptoms, especially in milder forms, e.g. CKD1-3. These stages of CKD may be picked up by a routine blood test. In this way it is initially a ‘silent disease’ – like high BP, cholesterol and early diabetes. Hence simply taking a medical history to make (or exclude) the diagnosis is not enough. You need blood tests.
Also many of these symptoms are non-specific, and can be seen in other conditions, like heart failure. The symptoms of CKD in males and females are largely the same. The causes of many CKD symptoms are not fully understood.
7. What treatment can the doctor offer? Alot. Does everyone with CKD need treatment? No
CKD is a spectrum, ranging from mild damage (CKD1-3) to advanced disease (CKD4-5) where the kidneys fail to work.
Even though CKD is not normally curable, there is alot doctors and the NHS can do.
Fortunately most patients have milder forms and will be able to control their CKD with lifestyle changes and regular medication review by their GP or practice nurse.
Others will need more treatment. This includes:
- Blood pressure (BP) tablets. Most patients with CKD have high BP. The treatment of high BP is more effective if you follow a low salt diet (see below). Talk to a dietitian or GP about that. Here is more information on how to lower BP.
- Angiotensin-converting enzyme inhibitors (‘ACE inhibitors’; e.g. Ramipril) or angiotensin II receptor blockers (‘ARBs’, e.g. Losartan) – are blood pressure tablets that have a special effect on the kidneys as they reduce protein levels in the urine, which is damaging. Ask your GP to be considered for one, if you are not taking one already. Most should be on one
- Sodium-glucose cotransporter 2 (SGLT2) inhibitor (e.g. Dapagliflozin) – are a newish class of diabetic tablets that reduce blood glucose levels by increasing urinary glucose excretion. But they have also been shown to be useful for many patients with CKD (and heart failure, CHF); especially if there is a lot of protein in your urine (with or without diabetes). Again, ask your GP if you are not on one.
- Specific treatments – for specific diseases exist, and are covered here.
- Diet. There is no such thing as a ‘CKD diet’. In the earlier stages it is OK to eat normally. Later on dietary restrictions or encouragements may be advised. A low salt and protein diet may help to control CKD symptoms. You may request being referred to a dietitian.
8. What can I do to help myself? There are THREE important things you should do
1. Know your numbers
Monitor these two numbers. The blood tests can be performed and monitored by your GP, but you can do a lot of this yourself.
- Creatinine blood test. This is the most reliable measure of kidney function; the higher the number the worse the kidney function. It should be below 120 mcmol/L
- eGFR. The creatinine level determines your eGFR and hence CKD stage – the higher the creatinine, and lower eGFR, the higher (i.e. worse) CKD stage [“Yes it is confusing” CKDEx Ed]. eGFR should be above 60 mls/min, ideally above 90 mls/min. You can chase these results via a website called Patients Knows Best (PKB). Registering with it is easy and free.
Note. It is also worth getting checked out for diabetes every six months. These things all tend to ‘go together’
2. Keep blood pressure down
Buy a BP machine from any chemist or large supermarket or Amazon – prices vary, approximately £20-£40. ‘A&D’ is a good make. Take your own BP once a week until stable.
Having normal (or better low) BP is the single most important thing for someone with CKD to do. Aim for 130/80 or below all the time (at home, GP or hospital).”

Get your BP checked. Better still buy your own machine and check it yourself.
3. Lose weight (if you are overweight)
For many patients with CKD, being overweight or obese is a major factor – as it causes diabetes and high BP. So, if requested by a doctor or nurse, please start to lose weight and it will help a lot.
Charity
Also, contact a major patient charity. Kidney Care UK is an important one. They can give you advice, especially on financial and employment issues, and give you grants – say for helping with the cost of dialysis (e.g. travelling) and heating bills. They have useful info like this on their website. There may be a local kidney charity called a Kidney Patient Association (KPA). See if you can find your nearest one.
9. How often do I need my eGFR/creatinine measured? – very variable
- CKD1-2, 3A – every 6-12 months
- CKD3B – 4 months
- CKD4 – 2 months
- CKD5 (dialysis or transplant). Very variable – from 2 weeks to 3 months
10. What is the outlook for CKD? – generally good, but very variable
- CKD stages 1-5 are very different, with different outlooks; generally the higher the level of CKD, the worse the outlook. Generally the outlook is good. Ask your doctor what yours is
- CKD does not always progress, e.g. CKD1 to 2, or CKD2 to 3 etc.
- The Kidney Failure Risk Equation (KFRE) can be used to predict your risk of the need for dialysis and transplant (CKD5).
Summary
We have described 10 CKD quick facts. We hope it has been helpful.
Other resource
Top Tip
If you are referred to a nephrologist (kidney specialist) make sure you have a kidney ultrasound. It often shows information that will help you.
Last Reviewed on 14 April 2024
