10 IBD (inflammatory bowel disease) facts
In this article, we will describe 10 inflammatory bowel disease (IBD) facts.
1. What is IBD?
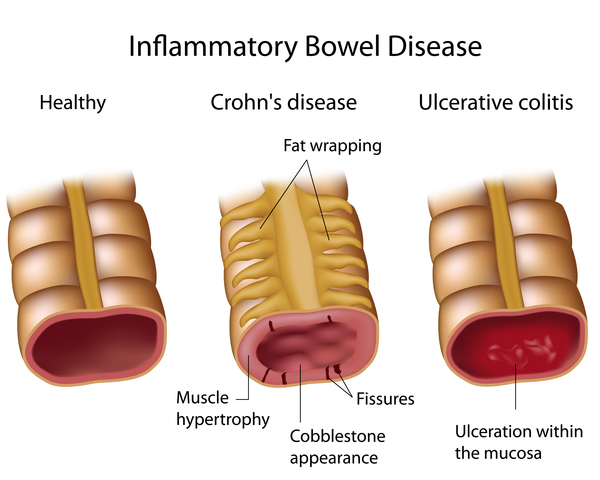
Inflammatory bowel disease (IBD) is a phrase for two long-term conditions – Crohn’s disease (CD), and ulcerative colitis (UC) – that are characterised by chronic inflammation of the gastrointestinal (GI) tract.
Ulcerative colitis is the more common type. It affects about 1 in 400 people in the UK. Crohn’s disease affects about 1 in 700 people in the UK.
 Gastrointestinal (GI) tract.
Gastrointestinal (GI) tract.
2. What are the risk factors for IBD?
- Age – most people are diagnosed with IBD before the age of 30 years, but IBD may develop in later ages as well
- Family history – you are at higher risk if you have a close relative such as a parent or sibling with the disease
- Cigarette smoking – is the most important risk factor for developing CD. Although smoking may provide some protection against UC, the overall health benefits of not smoking make it important to try to quit
- Oral contraceptives – increase the risk of IBD, particularly amongst women who smoke
- Non-steroidal anti-inflammatory drugs – NSAIDs such as ibuprofen and aspirin, may also trigger IBD
- Environmental exposures during rapid urbanisation – westernisation of diet, increased antibiotic use, pollution, improved hygiene status and early-life microbial exposure, have been shown to affect gut bacteria; which may trigger the immune responses that cause IBD.
3. What causes IBD?
The exact cause of IBD is unknown, but IBD is the result of an overactive mmune system. Possible causes are:
- The immune system responds incorrectly to environmental triggers, such as a virus or bacteria, which causes inflammation of the gastrointestinal tract
- A genetic component. Someone with a family history of IBD is more likely to develop this inappropriate immune response.
Diet and stress may make symptoms worse, but probably do not cause inflammatory bowel disease.
4. What are the affected areas of the bowel?
- CD: Can affect any part of the GI tract (from the mouth to the anus). Most often it affects the portion of the small intestine before the large intestine/colon
- UC: Occurs in the large intestine (colon) and the rectum.
5. How patchy is the damage?
- CD : Damaged areas appear in patches that are next to areas of healthy tissue
- UC: Damaged areas are continuous (not patchy) – usually starting at the rectum and spreading further into the colon.
6. What are the common symptoms of IBD?
- Mouth ulcers
- Persistent diarrhoea
- Abdominal pain
- Rectal bleeding/bloody poo
- Weight loss and fever
- Menstrual cycle change
- Fatigue.
7. How is IBD diagnosed?
- Blood tests – including a full blood count to check for anaemia, and blood tests to check for any indication of inflammation (called erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP))
- Stool samples – to check whether there is any infection in your intestines
- Scans – such as CT scan or MRI scan
- Sigmoidoscopy or colonoscopy – to look at the lining of your large bowel (colon) and to take biopsies (important to confirm the diagnosis).
8. How is IBD treated?
There is no cure for IBD, but it is often well-managed through medication and surgery.
Medication
Types of common medication to treat IBD:
- 5-aminosalicyclic acids
- Immunomodulators – e.g. Azathioprine, 6-mercaptopurine (or ‘6-MP’), Methotrexate, Ciclosporin and Tacrolimus
- Corticosteroids (steroids)
- Biological agents.
Some drugs are given as tablets, some as enemas (into the rectum) and some as weekly (or longer) injections.
Surgery
Surgery is used to remove damaged portions of the gastrointestinal tract.
Crohn’s disease
In fact surgery is common in people with CD. Most people diagnosed with CD will have surgery to treat their disease at some point in their lives. Approximately one-third of patients will have surgery in the first 10 years after diagnosis.
Ulcerative colitis
However the rate of surgery (usually colectomy, i.e. removal or part or all of colon) to treat the disease is low. It is approximately 10% at 5 years after diagnosis, and 15% after 10 years.
9. What are the complications of IBD?
Unfortunately having inflammatory bowel disease (IBD), or the medications used to treat it, put you at risk of developing complications and other conditions. These include:
Bowel
- Bowel cancer – if UC and CD is affecting the large intestine (colon)
- Fistulas – more common in CD than UC
- Intestinal abscesses – more common in CD than UC
- Intestinal strictures causing obstruction to bowel
- Bowel rupture
- Toxic megacolon – more common in UC than CD.
Non-bowel
- Vitamin and mineral deficiencies
- Bile acid malabsorption (BAM) – in CD affecting the small intestine
- Liver disorders – such as Primary Sclerosing Cholangitis (PSC)
- Loss of bone density and osteoporosis (steroids)
- Slow growth in children
- Joint pain and arthritis
- Pyoderma gangrenosum (and other skin conditions)
- Eye disorders
- Kidney disorders (caused by immunomodulator drugs)
- Anxiety and depression.
10. What is the prognosis (outlook) for IBD?
IBD is a lifelong condition. But, if the disease is mild, it should not shorten your life expectancy.
However it is quite difficult to state the ‘average prognosis’ for IBD; as it depends on a number of different factors, including the severity of the disease, the age at diagnosis, and how well the inflammation is controlled.
With proper treatment, you can prevent flares and have long periods of remission.
Summary
We have described 10 IBD (inflammatory bowel disease) facts. We hope you understand it better now.
Last Reviewed on 7 March 2024
