10 IHD (ischaemic heart disease) facts
In this article we will go through 10 top tips for ischaemic heart disease (IHD). Let’s start with the basics.

Coronary arteries
1. What is IHD?
Ischaemic heart disease (IHD), also known as coronary heart disease, occurs when the blood flow to the heart muscle is reduced because of a partial or complete blockage of the arteries supplying it with blood.
2. How common is IHD?
Ischaemic heart disease is common, affecting 5-10% of the population. Heart failure, which is usually due to IHD, affects 10% of the population. Also 20% of the population have high blood pressure (hypertension) that is linked to both.
3. What are risk factors for IHD?
- Age
- Smoking
- High blood pressure
- Hypercholesterolaemia
- Diabetes
- Family history
- Race (more common in non-Caucasians)
- Obesity.
4. What causes IHD?
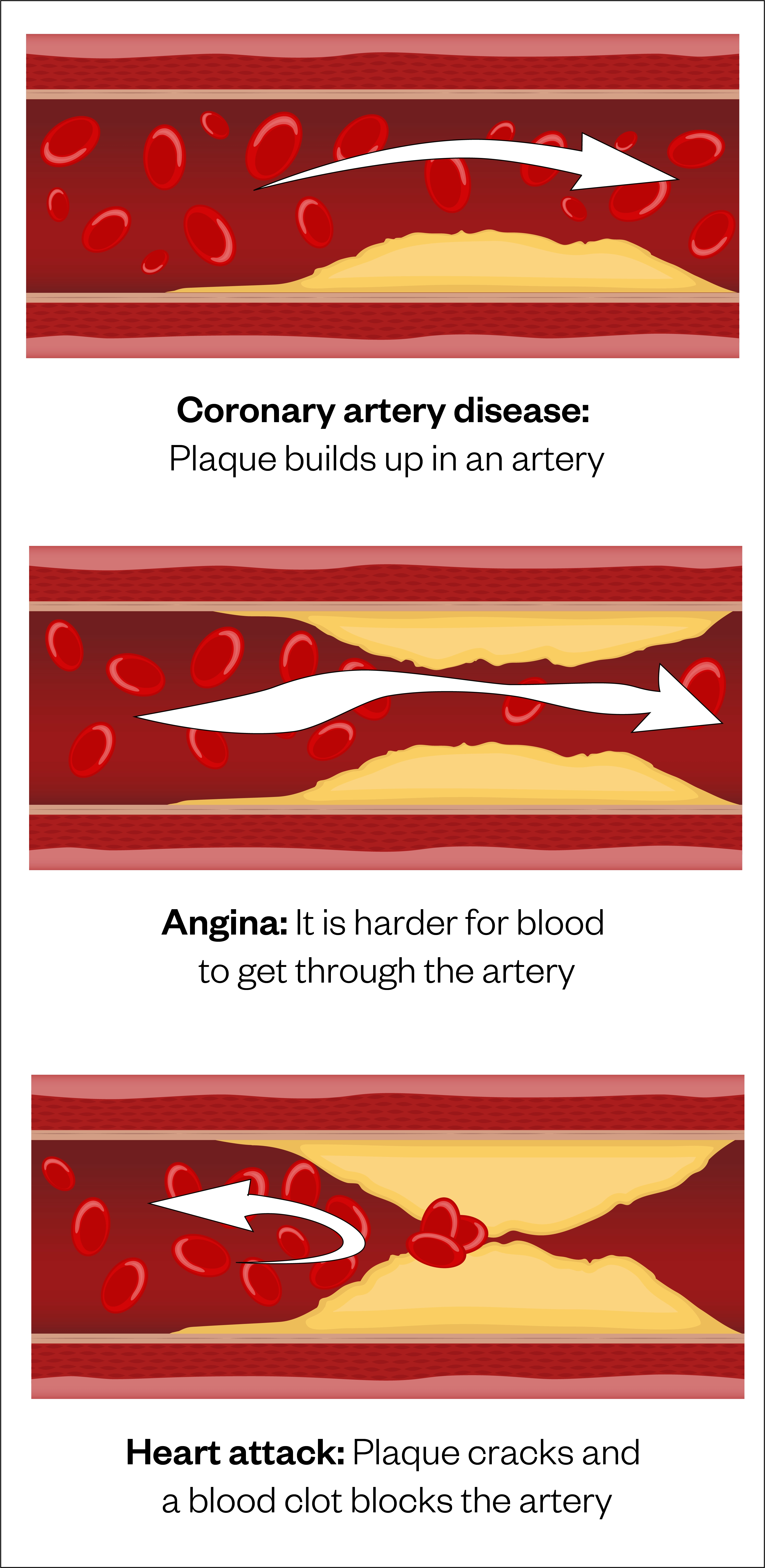
Ischaemic heart disease is caused by atherosclerosis. This is age-related chronic inflammation of the coronary arteries that supply blood to the heart muscle. It causes them to harden and accumulate cholesterol plaques on their walls. This is bit like a kettle getting furred up with chalk.
This leads to an increased risk of thrombus formation (blood clots attached to blood vessel linings) within the coronary arteries.
5. What are the symptoms of IHD?
IHD usually presents as chest pain, due to either angina (myocardial ischaemia) or a heart attack (myocardial infarction). It can also cause atrial fibrillation (AF; fast irregular heart beat); and acute and congestive (chronic) heart failure (CHF; weakness of the heart muscle). It can be the first presentation of AF or heart failure. These tend to present at fast irregular palpitations (AF) or shortness of breath (CHF).
6. Angina and heart attacks – what’s the difference?
Both cause similar chest pain – left sided that spreads to the left arm, jaw, neck or back. Angina is when there is partial blockage of a coronary artery. Whereas a myocardial infarction is when there is a blood clot blocking a coronary artery as shown below. Both are treatable.
7. How do I improve my IHD?
- Blood pressure. Buy a BP machine and take your own BP once a week until stable and below 140/90 every time, at home or the hospital. When stable, take it every three months
- Lifestyle changes. It is also good idea not to smoke, keep trim, exercise and keep your alcohol consumption down.
- New treatments and monitoring equipment. Talk to the health professionals below about these. Cardiac care is changing all the time, with new drugs, operations, procedures and electrical treatments appearing
- Charity. Contact a major patient charity, and join the local branch of that charity. The British Heart Foundation (BHF) is an important one. They have useful info like this on their website.
8. What can the NHS do to improve my IHD?
- GP. Many patients can be looked after by an NHS GP alone. But if things are not settling you should be referred to a hospital cardiology consultant
- Hospital cardiology consultant. Ask your GP to refer you to the local hospital cardiology unit (there will be one). Then when you see a consultant who specialises in heart disease, only let them discharge you when you feel that your heart condition is stable
- GP Practice Nurse. Many GPs have a practice nurse that runs a ‘long-term condition’ clinic (that includes IHD). Ask for three monthly review there until all the treatable things are under control (i.e. blood pressure, CKD, cholesterol, and diabetes if you have it). Some of them work with a clinical pharmacist who can fulfil a similar role
- Other diseases. It’s also worth asking your GP or practice nurse to check you out for diabetes, high BP. high cholesterol and CKD, every six months. These all tend to ‘go together’, and can contribute to IHD.
9. What is PCI (percutaneous coronary intervention) for heart attacks?
One of the most common reasons for admission to a coronary care unit (CCU) with IHD is a heart attack (myocardial infarction). Many patients with a heart attack need a percutaneous coronary intervention (PCI). This is a coronary angiogram/plasty, which is an x-ray procedure used to widen blocked or narrowed coronary arteries (the main blood vessels supplying the heart).
From the community, such a patient is taken to hospital and will often go straight to a ‘cardiac catheter laboratory (‘lab’)’ where the procedure is done, and then they are taken to the CCU.
10. What is the prognosis of IHD?
This is difficult to generalise about, as prognosis depends on which area of the heart is affected, and the chances of repairing damaged arteries. A large proportion of patients can, with appropriate treatment, eliminate the symptoms forever; whereas others may see their life expectancy reduced.
Summary
We have described 10 IHD (ischaemic heart disease) facts. If you do all of the above, you will get better care. This may help prevent (or improve) complications of heart disease, like heart attacks, angina and heart failure.
“Yes, it is confusing there are so many terms that relate to heart disease – e.g. angiogram, angioplasty, stent, cardiac, coronary, cardiology, cardiologist, ischaemic, IHD, congestive cardiac failure (CCF), coronary care unit (CCU), percutaneous coronary intervention (PCI) etc.” [CKDEx Ed”]
Other resources
10 CKD facts
10 CHF facts
10 diabetes facts
10 cholesterol facts
Last Reviewed on 27 May 2024
