Why is the case important?
Lupus nephritis (LN) is a complication of systemic lupus erythematosus (SLE) and can lead to end-stage renal disease (ESRD) and the need for dialysis and/or a kidney transplant.
There are five types of lupus nephritis (LN). They include membranous nephropathy (called Class V lupus nephritis) and a proliferative (rapidly progressive) glomerulonephritis (Class 3 LN). The first usually presents with nephrotic syndrome (and/or CKD); the latter usually as AKI (sometimes part of a pulmonary-renal syndrome)
Both types of lupus nephritis lead to kidney damage, and can lead to kidney failure – and the need for dialysis or a kidney transplant.
Anti-GBM disease (Goodpasture’s Syndrome) is a very rare, life-threatening autoimmune disorder that affects the kidneys; and is caused by the production of autoantibodies against the basement membrane of the glomeruli. The autoantibody attacks the Goodpasture protein, which is found in the basement membranes of the kidney and lungs. This is why it can also lead to an AKI episode and/or pulmonary haemorrhage (as part of a pulmonary-renal syndrome).
What happened in this case?
In this recent case (Sogbein et al, 2023), a 62-year-old Caucasian male presented with pulmonary nodules, a year-long rash, and tea-coloured urine. 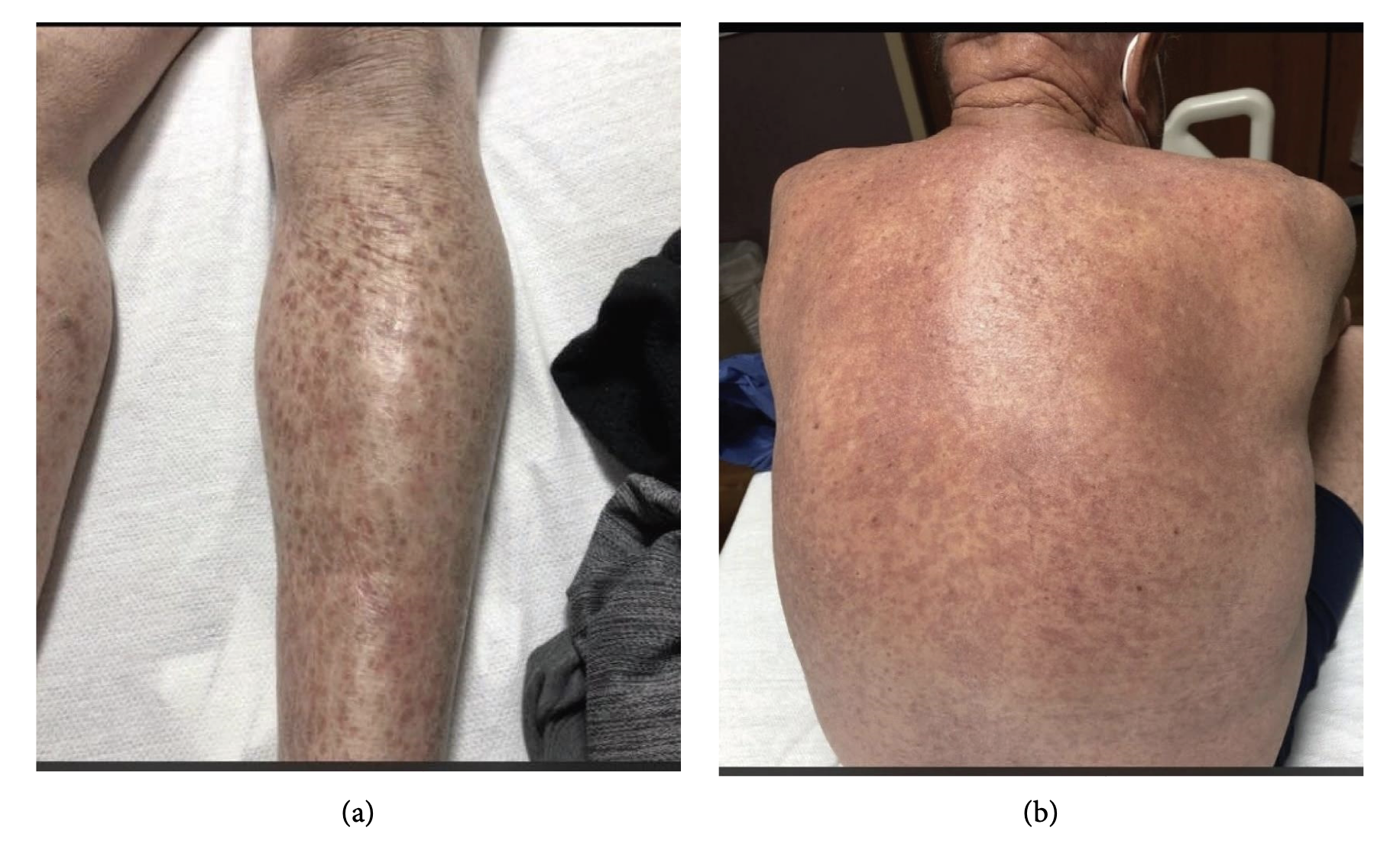 (a) The patient has purple spots on both arms and legs because of inflammation in small blood vessels. (b) The back side of patient’s chest and waist also have purple spots.
(a) The patient has purple spots on both arms and legs because of inflammation in small blood vessels. (b) The back side of patient’s chest and waist also have purple spots.
His laboratory tests revealed a creatinine of 194 mcmol/L, white blood cell count of 8.3 × 103 μL, haemoglobin of 128 gL, platelet count of 342 × 103 μL, normal liver function tests, and D-dimer of 1770 mg/mL. He was diagnosed with a prerenal acute kidney injury (AKI) and started on intravenous fluids. A week later, the patient experienced an episode of severe vertigo, nausea, and vomiting and was taken to the emergency department.
Urinalysis showed amber colored urine with 182 red cells with and 18 white cells. The patient’s protein/creatinine ratio (PCR) was 230 mg/mmol.
Over the next 48 hours, his creatinine increased from to 278 mcmol/L and a renal biopsy was performed. The patient’s complement levels were low (C3: 39 and C4: 2), urine and serum electrophoresis were unremarkable, cryoglobulins were absent, ANA titre was 1 : 20, and anti-dsDNA was 3.0 IU/mL. Furthermore, his IgG antiglomerular basement membrane (GBM) antibody was 63 AU/mL (normal 0–19).

Patient’s renal biopsy
A renal biopsy showed a combination of focal proliferative and membranous lupus nephritis (III + V). And a skin biopsy revealed the presence of a lupus band with deposits of IgG/IgA/IgM/C3/C1q at the dermo-epidermal junction, confirming the diagnosis of SLE.
The patient was treated with cyclophosphamide, corticosteroids, and therapeutic plasma exchange.
Later he began induction therapy with mycophenolate 500 mg twice daily, which was gradually increased to 3 grams daily in addition to prednisone (1 mg/kg). He responded well, with a decrease in uPCR from 230 to 30 mg/mmol over the next four months.
It was concluded that in rare cases, certain individuals may be predisposed to developing a combined LN and anti-GBM disease due to immune rearrangement or epitope spreading, likely due to anomalies in the kallikrein gene.
How does this affect you?
Generally, it does not. It is very unlikely that you will develop either of these uncommon serious illnesses. And the combination of the two is even more unlikely.
Nonetheless the fact that this combination is very unlikely can help you teach your doctors and nurses that in the world of kidney disease, rare things happens, sometimes at the same time. And so they need to have their antennae up at all times, and think laterally.
The cause of the combination of lupus nephritis and anti-GBM disease is not fully understood, but it is thought that the two conditions may share a common underlying mechanism. The autoantibodies in anti-GBM disease damage the basement membrane of the glomeruli in the kidneys, but could also lead to the development of lupus nephritis.
The treatment of the combination of lupus nephritis and anti-GBM disease is complex and requires close monitoring by a nephrologist. With appropriate treatment, most people with this condition can achieve a good outcome.
References
Sogbein, O., Kochar, T. and Afrouzian, M. (2023) ‘Epitope spreading: The underlying mechanism for combined membranous lupus nephritis and Anti-GBM disease?’, Case Reports in Nephrology, 2023, pp. 1–6. doi:10.1155/2023/3190042.
Last Reviewed on 25 September 2023
