Anaemia and chronic kidney disease (CKD)
Keep track of your kidney data with PKB
Anaemia means a lack of red blood cells in the body. The anaemia caused by CKD is called ‘renal anaemia’ and is largely caused by a lack of a hormone called erythropoietin (EPO).

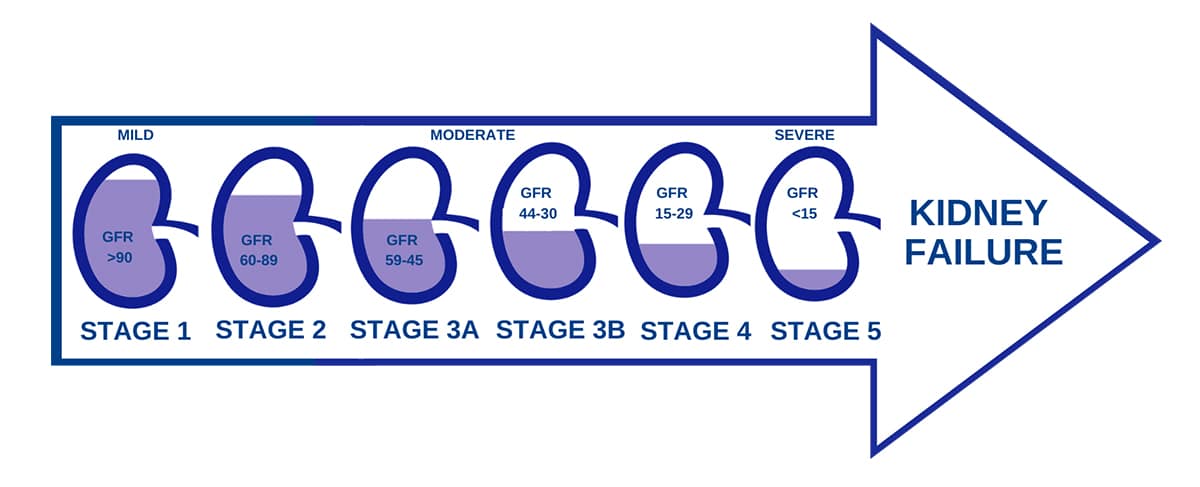
Fortunately renal anaemia largely affects patients in the more advanced stages of CKD, i.e. CKD4-5. Up until then it does not usually need to be monitored.
After then, in many patients, it should be monitored – using blood haemoglobin, iron, B12 and folate levels.
Let’s start with the basics about renal anaemia.
1. What is renal anaemia?
Anaemia means your blood is producing a lower than normal amount of red blood cells (RBCs). The function of red blood cells is to carry oxygen around the body.
Renal anaemia, also known as anaemia of chronic kidney disease (CKD) or anaemia of renal disease, is a common complication of people with CKD.
It is characterised by a decrease in the number of red blood cells, leading to less oxygen being transported in the blood.
2. What is the cause of renal anaemia?
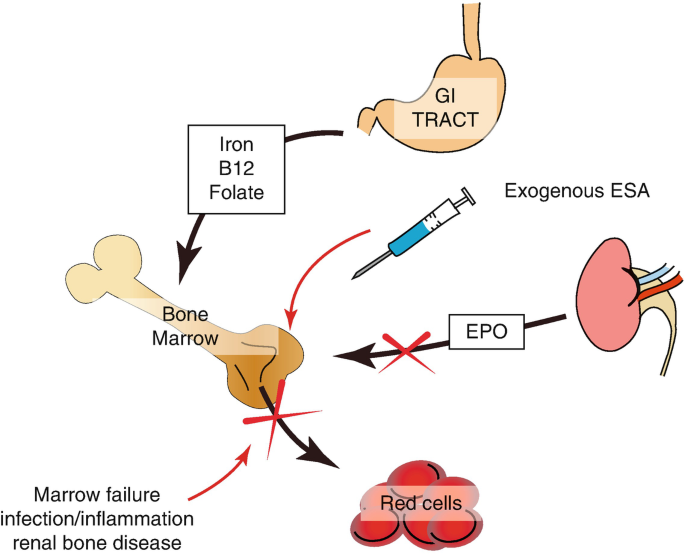
Renal anaemia is primarily due to the insufficient production of erythropoietin (EPO), a hormone produced by the kidneys that stimulates the bone marrow to produce red blood cells.
In CKD, the impaired kidneys fail to produce enough EPO, leading to decreased RBC production.
3. How common is renal anaemia?
Renal anaemia is very common. It is a frequent complication in individuals with CKD. Its prevalence increases as kidney function declines, with a significant percentage of patients experiencing anaemia in the more advanced stages of CKD.
Most patients with CKD 1-2, and CKD 3A, do not usually have anaemia. However, approximately 40% of patients with CKD stage 3B or 4 are anaemic.
The prevalence of anaemia increases to 75% in patients reaching CKD stage 5 (end stage renal disease, ESRD), i.e. those requiring dialysis or a kidney transplant.
4. What are the symptoms of renal anaemia?
Common symptoms include:
- Fatigue
- Weakness
- Shortness of breath
- Dizziness
- Pallor.
These symptoms arise due to reduced oxygen supply to tissues and organs.

5. How is renal anaemia diagnosed?
Diagnosis involves a blood test called a full blood count (FBC) to measure haemoglobin (Hb) levels.
Note: Haemoglobin is a protein present in red blood cells that binds to oxygen and enables it to be transported around the body.
Blood iron and ferritin (a marker of iron stores) levels are also measured.
Normal haemoglobin is 110-150 g/L in a woman, and 130-170 g/L in a man.
Therefore renal anaemia is diagnosed when Hb is <130 g/L for men, and <110 g/L or women – and CKD is thought to be the cause.
So, low levels of Hb in the presence of CKD indicates renal anaemia.
6. How is renal anaemia treated?
In accordance with NICE guidelines, management of renal anaemia involves addressing the underlying cause, which is primarily EPO deficiency.
To stimulate RBC production, and raise haemoglobin, EPO levels can be increased using:
- Erythropoiesis-stimulating agents (ESAs), like Darbepoetin alfa (given as an injection once a week)
- Hypoxia-inducible factor–prolyl hydroxylase (HIF-PH) inhibitors, like Roxadustat (given as a tablet three times a week).
The target haemoglobin is 110-120g/L in men and women. EPO is usually started when the Hb is under 100g/L.
7. Who should monitor renal anaemia and what should be monitored?
Managing renal anaemia requires a collaborative approach involving your nephrologist (kidney doctor), and specialist kidney nurse and pharmacist. The treatment is coordinated by the hospital team, not your GP.
They should monitor haemoglobin (Hb), iron, B12, folate levels – and adjusting doses of medication accordingly.

8. Is renal anaemia linked to iron deficiency anaemia?
Yes. Many CKD patients with renal anaemia also have iron deficiency, either because of decreased intake, impaired absorption, or increased losses.
Iron supplementation (as tablets or injections) may be requited to support the effectiveness of ESAs (like darbepoetin) and HIF-PH inhibitors (like roxadustat).
9. What is the impact of renal anaemia on quality of life?
Renal anaemia significantly impacts a patient’s quality of life by causing reduced physical activity, thinking ability, sex drive, and decreased overall well-being.
It is therefore a high priority to treat it, especially because it is easy to treat (unlike some other complications of CKD).
10. What are the complications of renal anaemia?
Untreated renal anaemia can lead to various complications, including strain on the heart, and reduced exercise capacity, amongst CKD patients.
Summary
We have discussed anaemia and chronic kidney disease (CKD). We hope it has been useful.
Other resource
Functions of kidney 5: blood cells, anaemia and EPO
There is more information on erythropoietin (EPO) written by the renal team at UHCW Coventry.
Last Reviewed on 17 June 2024
