Catherine’s Story: My journey to my living donor kidney transplant and recovery.
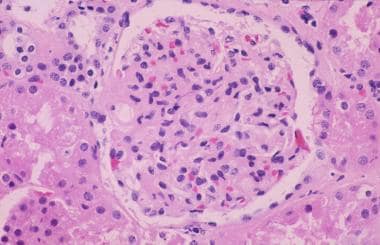
My diagnosis of Immunoglobulin A nephritis (IgAN) was made in February 1995. I had normal function back then and whilst there was a steady decline in my renal function over the years, I wasn’t anywhere near to conversations around kidney transplantation.
It is important to mention here that I am a qualified nurse (I was diagnosed with IgAN when I was training to be a nurse) and I worked for eight years on a haemodialysis unit in North Wales. I then moved over into education where I worked on the Pre-registration Adult Nurse Education Programme for ten years before moving into the Health, Mental Health and Wellbeing programme in 2015, where I continue to teach.
With all the experience I have gained, I always attended my clinic appointments with a professional view to my own kidney disease progression with the ability to access all the latest developments in renal nursing and transplantation. I had also worked as a nurse with my first consultant and registrar, so I had very much a different relationship with them that was not the usual patient/doctor relationship.
It wasn’t until 2020 that there was a noticeable drop in my kidney function. I was always aware this could happen, and I have considered myself to be very lucky that I had good function and was able to have my daughter whilst my function remained stable.
When I was at the clinic appointment with the registrar, whom I had a very good relationship with, she and I discussed the sudden fall in my estimated glomerular filtration rate and rise in my blood serum creatinine and urea levels. She felt I should see the consultant at my next appointment which was set at 3 months and not 6 monthly, which I had been used to.
To be honest, I still wasn’t too worried at this point as I still felt well. I may also have felt a lack of worry as I knew the process well and understood the implications of the decline in my function. I also knew I wasn’t at the point where I needed to be referred for a transplant or dialysis.
The following 18 months saw my function decline to the point where my consultant and I discussed transplantation and dialysis. I was still under 50 and in good general health. We both agreed a pre-emptive transplant (where you receive a kidney before you go on dialysis) would provide me with the best outcomes for my clinical health, mental health and wellbeing.
I was referred for the various transplant work up tests that included cardiac scans, and ECG and cardiorespiratory resistance test (where you cycle on a static bike and resistance is added and your cardiac and respiratory function under exercise is tested). There was a cause for concern following the results of my cardiac echo which suggested I was developing heart failure, yet my exercise resistance test suggested the opposite and I was in very good cardiac and respiratory health.
I have to admit; the cardiac echo results did worry me, but this all changed after the exercise stress test. I spend a lot of time dancing and doing fitness classes (which are my go-to to unwind and de-stress) and I was worried I wouldn’t be able to do as much as well as being declined or classed as a high risk for surgery. However, with all the results completed and with them demonstrating I was a very good candidate to receive a transplant, I was referred to Liverpool; my local transplant centre.
I knew my best option for a pre-emptive transplant would be from a live donor as this process tends to be a lot faster; taking anywhere from 4 -8 months. Whilst there is the transplant list patients can be registered on, the wait for a cadaveric kidney is unpredictable and can be a wait of several years. I felt I didn’t have that time to wait so I actively approached my close and wider family members in the UK and the USA. In the end, two cousins came forward to offer me one of their kidneys. One living in the UK near to Liverpool and one in Maine, USA. I gave both names to the transplant nurses at my renal clinic and then they sent out the relevant documentation and informed Liverpool I had two potential live donors before my first appointment there.
I didn’t go alone to my first appointment with the transplant surgeon. I took a friend and colleague; also a nurse, but with a surgical background. I was apprehensive about going to this appointment alone which felt alien to me. I happily attend all my renal appointments with my usual team alone. I have done from the very start. Yet this felt bigger, different and unknown and I felt I needed support.
I was very much out of my comfort zone. Both my friend and I reflected on this as we both felt that entering the NHS as a patient with prior working knowledge offers a different perspective and different vulnerabilities.
This is hard to explain in words. All patients undergoing treatment are vulnerable, but I hadn’t experienced this from a personal perspective until this point. I was lucky that my surgeon was a gentleman and respected both our knowledge and still gave time for both of us to ask questions. I was glad I had brought another nurse with a different background along with me as she asked questions I wouldn’t have thought to have asked due to my own prior knowledge and experience.
My surgeon was aware I had two living donors. I was concerned they wouldn’t consider my family member in the USA, but he eased my worries as he informed me that the Atlantic was not a barrier. He did state that they would most likely start with my family member living in the UK as it was easier.
I was listed on the UK transplant waiting list in May 2023. Discussions were ongoing between my family member in the UK and, after meeting with the transplant nurse in Liverpool in June 2023, he agreed to become a live donor. His work-up started in September, and he was found to be a 50% match to me, so they continued with the process. I was aware that with each test, he could be found to be not a candidate for a donor. Fortunately, his work up all went well and he was physically fit and well enough to offer me one of his kidneys.
In January 2024 we finally attended clinic at the same time, but seen separately. We were offered a date in February, but as glucose was found in his urine test at that clinic, he needed to undergo another test to see if he had a health problem that had been missed. We were both worried about this development. My cousin actively changed his diet to include less sugar and more nuts. I worried this would stop the process and I was getting very close to needing dialysis, and I had already been referred for a PD tube. It did put the operation on hold, but only by one month and it was rescheduled for March.
Fortunately, his test results came back normal, and the March date went ahead and at our pre-op clinic, all was fine.
When I was finally admitted, I felt very strange. It’s hard to be a patient when you can see all the nursing jobs that need to be done. I also had very high expectations of what my nurses who were caring for me should be doing. I was impressed with the nursing team and I felt their levels of care met my expectations most of the time I was an inpatient.
On the day of the transplant, I was more worried about my cousin than myself. I just wanted to know he was safely though his operation and there had been no complications for him. It didn’t cross my mind to think about the kidney at this point. I was just very worried about what I had asked of him. At the end of the day, he did not need surgery. He was offering to undergo surgery to donate his kidney to me. I was fully aware of the gift this was, but I felt concern for his health as he really didn’t need to do this. But I was so grateful. All went well though and I eventually was sent to theatre.
When I woke up, I instantly wondered what the hell I had done. I had gone to theatre feeling ok and in no pain. I woke up feeling instant pain in my abdomen, a mouth drier than the desert and began to feel very sick (as it turns out, intravenous morphine doesn’t agree with me.) I also felt very full of fluid. The only thing that helped, was that the kidney was already working and I was producing large quantities of urine and I actually needed a lot of IV fluid to maintain my fluid balance.
Within twelve hours of surgery, my renal bloods were already improving with my urea and creatinine falling and my eGFR rising. The only problem was the nausea and vomiting and lack of appetite. Even when the IV pain relief was stopped, I still felt sick and my appetite wasn’t great. I survived on cheese and crackers then finally bread and cheese. But despite that, I was starting to feel different. According to my family and my cousin who kept popping over to see me, I was looking better despite me feeling very nauseated.
It was in those early days, following the transplant, that I realised how poorly I’d become. I could see a difference in my skin tone; the greyness to my skin was gone. The main challenge I had was to drink 5 litres of fluid in a 24-hour period, to get rid of the nausea and to get my appetite back.
My cousin was doing well though, and he was discharged quickly post op and I was glad he was doing so much better than I was. I had to stay in for seven days, which felt too long, but I was in the right place as I had been so poorly with nausea, home wasn’t the best place until that passed. Once home, I did start to feel better. I was sleeping better, and I was walking around a lot more and slowly my appetite was returning. The trips to clinic were regular, but luckily Liverpool transplant nurses discharged me back to Wales, so I had less distance to travel in the second week of being home.
My wound healed quickly which led to a slightly early removal of my clips which I was glad to see the back of. My renal bloods continued to improve and I was back driving at 3 weeks and at 8 weeks post op I was finally back dancing and straight into rehearsals for our dance school’s show.
Having dancing back in my life and three dances to learn in six weeks meant I had something to focus on and my daughter was also representing the dance school with the rest of the competition team, as they were part of Team Wales and had danced through to the Dance World Cup that was taking place in Prague.
Prior to my transplant we knew this was happening, but we hadn’t booked flights or accommodation. We also needed to renew our passports. Pre-transplant, I hadn’t felt this was something we needed to do. My focus was on the operation. Even post operatively, the need to book everything still felt strange. After much nagging from my partner and other mums who were also going to Prague we booked, and I reflected on my reluctance to book anything. I think I had stopped planning anything for the previous 2 years. I had put my life on hold. I couldn’t see a future, so why plan? I had just been getting through each day. I am a positive person, and I remained positive right up to my transplant, but all of my effort was going into just surviving and maintaining my work ethic. That left no room to plan for a future I couldn’t think about. I have found it hard to change that outlook, but I am getting better.
There aren’t the words in the dictionary to say how grateful I am to my cousin. It has brought us closer. I am so proud to call him my cousin and my donor. He has given me a renewal for life. I was performing on the stage 14 weeks post op and I am back in the adult competition team, and we are performing next month. Yes, the op was hard, recovery in the first month was hard and painful, but it’s worth it.
I feel well and ready for the next thing life throws me.

Last Reviewed on 24 September 2024