Common medication errors (and how to reduce them)
Prescribing errors are the second most common type of medical error (after communication).
Information in this article can save a patients life
All good doctors are good prescribers. Bad prescribers are dangerous
In this article we will describe common medication errors (and how to reduce them)
Why are medication errors important?
Medication errors can have anything from minimal/no to severe effects (including causing or contributing to death, permanent dialysis, loss of limb and blindness). 30% of hospital admissions are due to (or in part due to) prescribing errors.
We will now go through the most important ones.
Wrong dose
This can be anything from a:
- Minor mistake – e.g. 10mg Bisoprolol OD when 5mg was intended, to a ..
- Major mistake – when 1000x dose is given, e.g. if a drug normally in mcg (alfacalcidolol) is written up (and given) in mg.
How to reduce error
As a prescriber, you should know the dose range for any drug you are giving, and know the one that you want for that patient. You should be careful with the units used, e.g. g, mg, mcg, pcg etc. If you are not sure look it up in the BNF (British National Formulary). This incorporates NICE guidelines.
Does adjustment for CKD, CLD, size or age of patient
E.g. allopurinol should be 100 mg OD, not 300 mg OD, in patients with CKD.
Wrong frequency
There is a wide range of frequency of drug prescribing. Drugs are commonly given anything from 4x/day (qds; some antibiotics) to once a week (erythropoeitin, EPO).
How to reduce error
You need to know the correct frequency for the drug you are prescribing. Again, if you are not sure, look it up in the BNF.
Wrong length of course
There is a huge range in terms of the length of a course of a drug – from one dose (e.g. a high dose of an antibiotic) to long-term (i.e. until your doctor says stop taking the drug).
How to reduce error
You need to know the correct duration for the drug you are prescribing. Again, if you are not sure, look it up in the BNF.
Wrong drug
This is surprisingly easy. There can be a wide range of errors.
- Minor – for example, drugs with similar names (e.g. dapagliflozin and canagliflozin). Even though these drugs are in the same group (SGLT2is), the correct dose if very different: dapagliflozin 10mg OD vs canagliflozin 100 mg OD. So, it is easy to prescribe a very incorrect dose in a similar drug. Hence a drug error that seems minor is actually significant.
- Major – this can happen when drug names are similar, e.g. diazepam, diltiazem and digoxin (latter two are cardiac drugs). Others drug pairs with similar names include metformin and metronidazole; and hydroxyzine and hydralazine.
How to reduce error
This is largely a matter of knowledge and experience. But, if handwritten prescribing is used where you work, your handwriting is important too. This is why drug names should always be written in CAPITALS.
Note. The right drug can also be given to the wrong patient. This happens especially on busy wards with patients with similar (or sometimes identical) names, dates of birth (it happens, yes) or diseases (everyone has diabetes, heart failure, CKD, high cholesterol and hypertension). You need to put a reminder in the notes, and by the patient’s bed; to remind staff that this possibility is more likely with these two (or more) patients. Move patients with very similar names.
Known allergy
Drugs allergies are common. You need to distinguish between a minor rash and a potential anaphylactic reaction. For example if on the last occasion the patient received a drug (say a penicillin) their face became swollen and they became wheezy, the next dose could lead to an even more serious reaction. If in doubt, use a different drug.
How to reduce error
Ask the patient, look at hospital and/or GP records. If you are not sure, ring the patients family. Check check check. Unfortunately hospital, GP and pharmacy computers are not linked up. So the absence of a drug allergy on one means nothing.
Drug not given, or given more than once
This is surprisingly common. Why? Many reasons. For example, the patient may be away from their bed on a drug round. Or two nurses give a drug dose as each thought the other had not done it.
How to reduce error
Check the drug card carefully every day, making sure all the prescribe drugs are being given. Or, if they are not given, has the nurse indicated why not given? It may be important eg antihypertensive not given as BP 80/40 – i.e. you may need to stop or reduce dose of that drug.
Illegible writing
This is an unforgiveable mistake. It is not funny that doctors seem to think that it is a laughing matter, and they ‘should have’ bad hand writing.
Band handwriting is lazy and lethal. Do it properly. It is not funny
How to reduce error
Write neatly, clearly and professionally from a position of knowledge, experience and care. Full stop. Write in CAPITALS if necessary. The drug name should be written in capitals anyway.
How to write up a drug properly
These are examples of moderately good prescribing.
Hand-written
Note. This is quite good. Spot any mistakes? Yes:
- The signature is unclear. If yours is a ‘squiggle’ like this, change it. Use your surname in capitals if needed
- The dose of FUROSEMIDE (in mg) is too near to the number, eg a ‘u’ in ‘ug’ can be too similar to a ‘0’.
Computer-generated
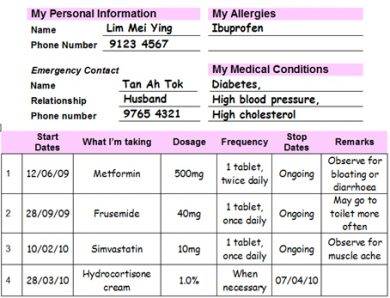
Note. This is clearly computer generated. If it was handwritten it should be of the same standard. It is not perfect. Can you see errors? Yes, no capitals and who is prescribing these drugs?
Summary
We have described common medication errors (and how to reduce them). We hope it has been helpful.
Other resources
British National Formulary (BNF)
How to reduce prescribing errors (shorter article)
3 top prescribing tips (even shorter article)
CKDEx’s 3 Top Prescribing Tips
- Use one drug in each drug category, e.g. dapagliflozin OR canagliflozin – and know the standard dose and frequency of that drug, dose adjustments (e.g. in CKD) and when not to use
- Buy a clinical pharmacology textbook (paper or cyber) and keep it near you (and use it) when at work
- Read the BNFs guidance on good prescribing regularly (and follow them): https://bnf.nice.org.uk/medicines-guidance/guidance-on-prescribing/.
Last Reviewed on 19 April 2024
