Debates in nephrology: CKD staging system
Introduction
In 2002, the US National Kidney Foundation (NKF) released a new classification of chronic kidney disease (CKD) (Levey et al, 2003).
This classification system represented a new conceptual framework for the diagnosis of CKD, moving away from an diagnosis-based system to a scheme based on disease severity defined by glomerular filtration rate (GFR).
The introduction of the CKD staging system stimulated significant interest in kidney disease, increasing CKD research, placing CKD on the public health agenda, and increasing awareness of CKD at both the population and individual level. This was a good thing.
Purpose of CKD staging system
The system was created for three reasons:
- Primarily, it is meant to aid identification of individuals at increased cardiovascular and dialysis risk; and to help improve the treatment of patients with CKD – and thereby ideally to prevent (or at least delay) dialysis
- To reduce the underdiagnosis of CKD, when based on blood creatinine alone
- To become an international language to define and classify CKD. This is especially useful in research.
But. There is always a but. We will expand on ‘the but’ later. First of all, what is the current system?
Current CKD staging system
Before discussing the controversies with the current CKD staging system, it is important to provide detail on the current CKD classification. We will start with a current definition of CKD.
Definition of CKD
- An estimated or measured glomerular filtration rate (GFR) of <60 mL/min – that is present for at least three months with or without evidence of kidney damage; or,
- Evidence of kidney damage with or without decreased GFR – that is present at least three months, as evidenced by albuminuria (protein in urine), haematuria (blood in urine, after exclusion of urological causes), structural abnormalities (e.g. on renal ultrasound) or pathological abnormalities (e.g. on kidney biopsy).
Note. In some milder cases of CKD there is evidence of kidney damage but normal renal function (normal GFR/creatinine).
This is a simplified version but does emphasise the need to show kidney damage in CKD1-2 to diagnose CKD.
As can be seen from the definition above, the modern system has four components:
- An anatomical or structural component (kidney damage)
- A functional component (GFR)
- A temporal component (the abnormalities must be present for more than three months)
- And now .. a presence/absence of urinary albumin (and level). This was not an original part of the CKD stage system.
In the majority of cases, the functional component based on GFR is estimated using an estimated GFR (eGFR) equation. There are a few equations which can be used. The original equation was the Modification of Diet in Renal Disease (MDRD) study equation. Currently the CKD-EPI equation is recommended.
According to the classification system, someone is diagnosed with CKD if they have evidence of kidney damage (and GFR 60-90 ml/min, i.e. CKD stage 1-2) or an estimated GFR (eGFR) <60 ml/min (CKD stage 3-5). Kidney damage is defined as the presence of pathological abnormalities or markers of damage including abnormalities in urine tests (albuminuria) or imaging studies (e.g. ultrasound diagnosing PCKD).
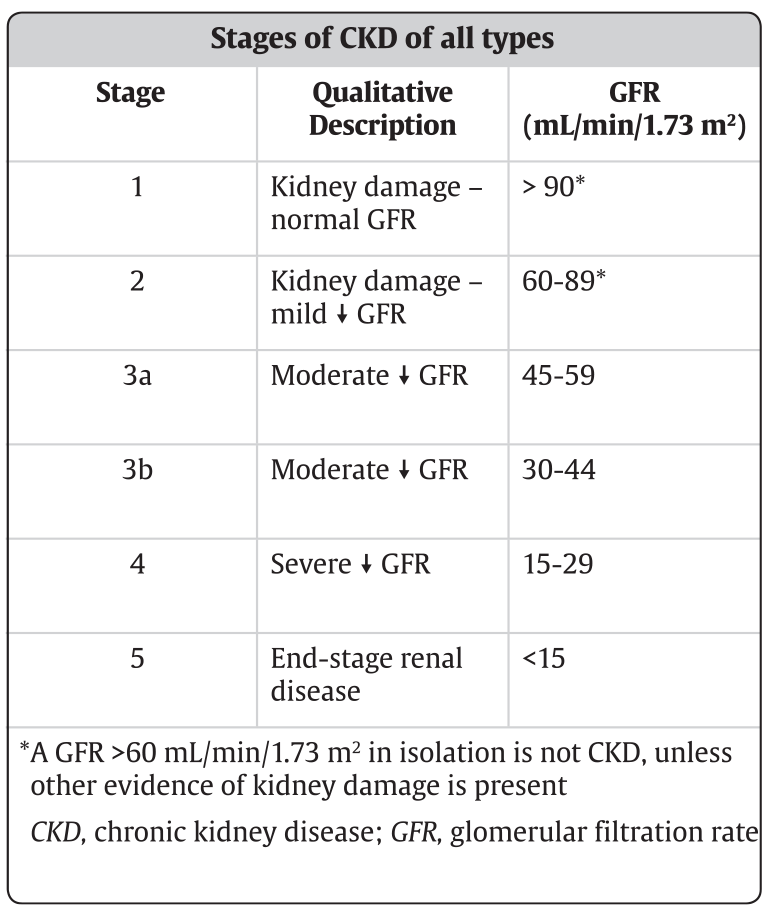
Once diagnosed with CKD, the severity is classified in five stages based on the level of kidney function defined by the GFR. The temporal component states that the abnormalities must be present for more than three months – i.e. GFR must be measured at least twice in 3 months, and both are ‘below the line’.
CKD stage and urine ACR (protein level)
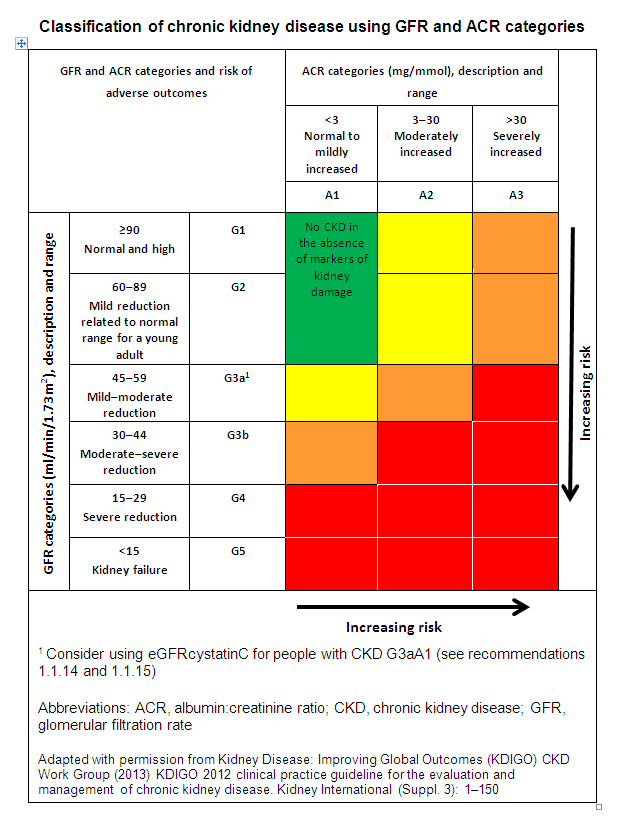
Just to make things more complicated we now describe CKD not just via GFR but also add the level of protein in the urine (called the urine ACR, uACR).
Urine ACR is combined with the CKD stage (Grade or ‘G’ 1-5) to estimate the outlook for someone with CKD as a higher level of albumin in the urine is often associated with a faster deterioration in kidney function.
Controversies in the CKD Staging System
The concerns regarding the current CKD Staging System can be grouped into the following areas.
1. Methodology
A first major criticism with the CKD Staging System has surrounded the accuracy of the eGFR estimates using the MDRD study equation. It was developed as a research tool, in a population with CKD that may not be typical, and there have been legitimate concerns regarding the imprecision and bias of the equation to estimate true GFR. For example, it is clear that as (true) GFR increases above 60 ml/min, the equation underestimates the GFR, leading to an overdiagnosis of patients with CKD.
Before the advent of the CKD Staging System, when CKD (or chronic renal failure (CRF) as it was called then) was diagnosed by the blood creatinine level alone, there were similar concerns ‘ the other way’. In other words, just measuring the blood creatinine, made us miss many patients with significant CKD – and a risk of dialysis (that could be prevented).
2. Over-diagnosis of ‘CKD’
The second major criticism of the CKD Staging System was the definition of chronic kidney disease as an eGFR<60 ml/min (CKD3 or worse), without the need for proof of any other measure of kidney damage such as proteinuria, haematuria or abnormality on renal ultrasound. These are needed to diagnose CKD1-2, i.e. in its earlier stages.
Hence less than careful doctors (and increasing A1-type computers!), may over-diagnose CKD (or not) based on a single number (GFR based on a blood creatinine) – without seeing, examining and investigating the patient properly. Also they may not be careful enough to measure GFR twice, 3 months apart, that is needed to make a diagnosis.
This is especially true in research studies of large numbers of patients where checking of the diagnosis is hard.
Major general population epidemiological studies, such as those derived from the NHANES Survey in the US, described a surprisingly high prevalence of CKD (of just under 8%) (Coresh et al, 2007).
“These and other studies have led to the widespread belief that CKD affects 10% of the world population. This may be untrue”
Of particular concern in NHANES was the high prevalence of ‘CKD’ (30-40%) in the elderly. These estimates were largely driven by subjects (especially females) with an eGFR of 45 to 59 ml/min (‘CKD3A’), without proteinuria. Therefore ..
“Many nephrologists consider that a large number of these older people are in fact normal, with the eGFR values representing the ‘normal’ age-related decline in renal function, and they have questioned the automatic labelling of this group as having CKD.”
.. and ..
“Hence there are concerns regarding whether all of CKD stages 1-2 and stage 3B should be termed a ‘disease’ – the term ‘risk factor’ may be better”
3. Appropriateness of thresholds or cut-offs for CKD Stages
The current CKD Staging System divides people with kidney disease into pre-defined stages according to eGFR. The separation into stages is based on severity, and is inherently arbitrary. For example the ‘cut-off’ between CKD2 and CKD3A could just as well be 55 ml/min or 65 ml/min – not 60 ml/min.
The presence of microalbuminuria is currently sufficient to diagnose CKD stages 1 and 2. Whether microalbuminuria truly represents kidney damage or just reflects inherent vascular disease has also been debated.
However, it is clear that albuminuria, whether micro or macro, is not just a potent cardiovascular risk factor but also independently predicts the development of end-stage renal failure (ESRF), and dialysis.
It is also true that 10% of the population have microscopic haematuria. And this can be part of a diagnosis of ‘CKD’. As with patients with microalbuminuria which ‘qualifies them’ for having CKD, such individuals may not have a chronic kidney disease at all – and are therefore not ‘patients’ or have ‘CKD’.
4. CKD diagnosis (cause of CKD)
According to the current staging system, a person has CKD if they have evidence of kidney damage (with normal or near normal kidney function), or an eGFR of <60 ml/min with or without kidney damage. There is no consideration given to diagnosis (cause) of CKD in the current system.
Many nephrologists are uneasy about the lack of consideration of pathology in the ‘diagnosis’ of CKD. They are concerned it will lead to diagnostic laziness. This is similar to diagnosing ‘anaemia’ as a disease and treating it with iron tablets, or ‘heart failure’ and treating it with diuretics. Like CKD, anaemia and heart failure are syndromes, with different diseases causing them.
“CKD is not a diagnosis. It is a syndrome with different diseases causing it. The precise cause should be found, as it affects treatment”
5. Over-simplification of CKD stage system
All of the above leads to authors producing tables such as this one:

Such tables are a. hugely over-simplified, and (therefore) b. wrong.
“They may lead to a generation of junior (and especially student) health professionals with false ideas of what is CKD, how to define it, and a lack of care and precision re the underlying diagnosis (cause).”
Some things to explain to patients:
- “‘Chronic’ doesn’t mean ‘really bad’ as many lay people think. ‘Chronic’ just means longstanding (as opposed to ‘Acute’, which also doesn’t mean ‘really bad’ but actually means ‘short-term). Patients can have Mild Chronic disease or Severe Chronic disease, or anywhere in between
- We developed the CKD system 20 years ago – and whilst I think it has been really helpful most kidney doctors would have made some changes if we could go back in time and design it again. Such as:
- Changing the thresholds of what is Stage 3, 4, etc. Because people are aware of Cancer staging and know that Stage 3 cancer is often really quite bad, whereas many people with CKD Stage 3 (especially earlier stages, what we now call Stage 3a) have a very mild disease (which will never reach kidney failure) – and may not impact on their health or life expectancy at all
- Narrowing the threshold of what we call Stage 3 (which we wouldn’t have called stage 3!) – as it covers far too wide a group of people
- But even though I don’t expect your kidneys to give you any future problems – e.g. in a patient with an eGFR of 50+ with no albuminuria or other risks for progression for their age – the fact that you have been ‘labelled’ as having CKD gives us the opportunity to monitor it regularly in future to reassure us that it is indeed remaining stable
- The monitoring of blood (and urine) tests is really helpful – in patients who have been labelled as having (or being at risk of having) CKD because there are usually no warning symptoms which is why many people used to get to kidney failure unexpectedly.”
Consensus view
The CKD Staging System has helped nephrology and transplantation in many ways. It has created an international language; stimulated research; reduced under-diagnosis of CKD (albeit by creating over-diagnosis); provided the impetus to standardise serum creatinine assays across laboratories and countries; and developed increasingly accurate GFR estimating equations.
These are all good things. The majority of nephrologists would acknowledge the important advances seen since the classification system was introduced in 2002.
[“.. so I guess that’s the CKDEx view.” CKDEx Ed] (sure is)
Summary
We have described the debate in nephrology regarding the CKD staging system. Overall, we think it has done more good than harm by identifying (and often preventing kidney failure) in a huge number of patients who would not have done so under the previous ‘CRF system’. We hope the article has been helpful.
This article was reviewed by Dr Dan Ford, Consultant Nephrologist.
Last Reviewed on 16 April 2024
