Why is this case important?
Nephrotic syndrome is rare, as is bilateral retinal detachment. When two unusual things happen at the same time (especially in different body systems), you should always ask yourself ‘are they connected?’ Also, a rapid diagnosis is required when permanent visual loss is a possibility.
What happened?
In a recent case report, Ye et al (Front Neph, 2023) described a 54-year-old woman (a professional dancer) with minimal change nephrotic syndrome who presented with sudden-onset of visual blurring in both eyes. Optical coherence tomography scans revealed retinal detachment. A kidney biopsy confirmed the diagnosis of minimal change disease. Steroid therapy was quickly started. During remission, her vision was restored, with complete resolution of the subretinal fluid observed on optical coherence tomography.
Their conclusion was, in minimal change nephrotic syndrome, fluid accumulation in the retina layer may occur, and gravity-induced vitreous traction on the inferior retina may cause retinal detachment. Patients should be advised to avoid large swings of the head and neck, handstands, and other activities that may increase the risk of retinal detachment. The possibility of retinal detachment should be considered when blurred vision occurs.
How does it affect you?
It does not. The likelihood of you having these two rare conditions at once is staggeringly low – and being a dancer! But this case demonstrates the principle of Occam’s Razor which is important in medicine. This states the ‘simplest explanation is the most likely’, i.e. if two (or more) unusual things happen at once, one cause is more likely than two (or more). You can help your doctors by reminding of them of this principle.
These are the patient’s optical coherence tomography scans (both eyes).
Before steroids
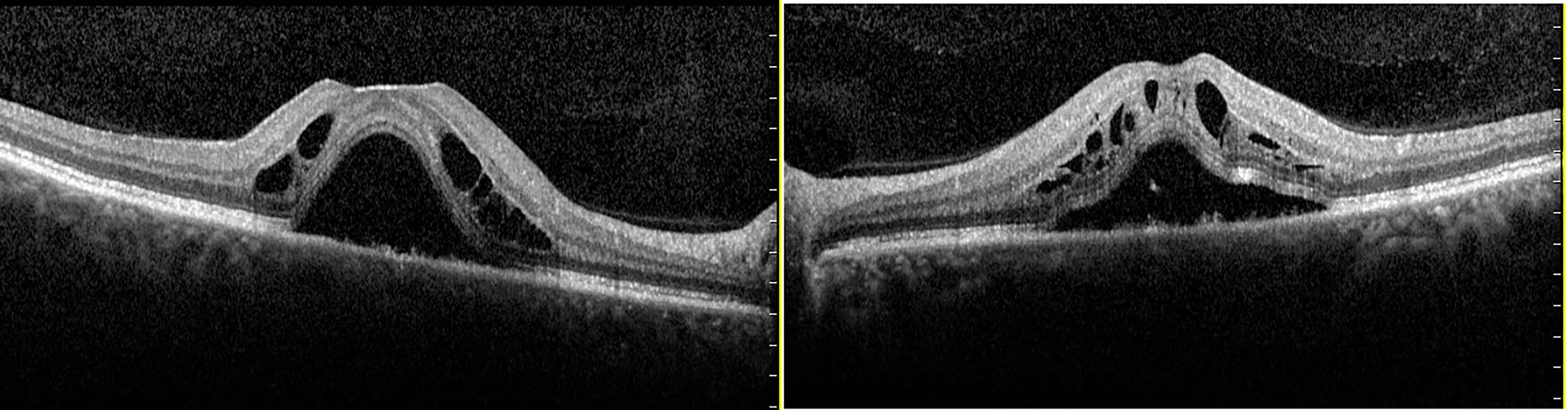
After steroids

Last Reviewed on 18 September 2023
