E Coli O145 outbreak in UK – HUS and AKI
Public health agencies across the United Kingdom are searching for the source of an Escherichia coli (E Coli) outbreak which has affected more than 100 people in less than two weeks.
E Coli is a common bacterium. It is a common cause of UTIs and sometimes gastroenteritis. It does not always cause disease.

E Coli bacteria
Shiga toxin-producing Escherichia coli (STEC) is a bacterium associated with food-borne diseases. And the STEC O145 serogroup can cause a severe gastroenteritis causing acute watery and bloody diarrhoea, haemorrhagic colitis, and haemolytic uremic syndrome (HUS).
There have been 113 confirmed cases in the E coli (STEC) O145 outbreak since May 25th 2024. This E Coli (and other forms) can occur after eating undercooked meat or unpasteurised milk.
The UK Health Security Agency (UKHSA), Public Health Scotland, and Public Health Wales are investigating the outbreak.
UKHSA warned that confirmed cases will rise as further samples undergo whole genome sequencing. Typically, the UK sees about 1,500 STEC infections per year.
We will now discuss the current E Coli O145 outbreak in the UK – and explain how it may cause HUS (leading to AKI).
Current E coli (STEC) O145 outbreak
At present, 81 people are sick in England, 18 in Wales, and 13 in Scotland. Northern Ireland has one patient who likely acquired the infection in England.
Patients range in age from 2 to 79 years old, with the majority being young adults. Of the 81 cases in England, 61 have provided information to UKHSA on food, travel, and potential exposures, and 37 people have been hospitalised.
Whole genome sequencing of samples indicates that most cases are part of a single outbreak. Based on the wide geographic spread of sick people, it is likely that the outbreak is linked to a nationally distributed food item or multiple items, said UKHSA.
The Food Standards Agency (FSA) and Food Standards Scotland (FSS) are also involved in the outbreak investigation.
There is no connection with the E coli O145 outbreak reported earlier this year, which was linked to raw milk cheese produced by Mrs Kirkham’s that sickened people in England and Scotland.
About E. coli infection, food and animals
E coli infections can occur after eating contaminated food, such as undercooked meat, drinking unpasteurised juices or dairy products, or being in contact with cattle and other farm animals or with a person who has the infection. This is why outbreaks occur in children visiting petting farms.
Food contaminated with E coli does not usually look, smell, or taste spoiled. Anyone can become sick with an E coli infection. Infants, children, the elderly, and people with weakened immune systems are at higher risk of serious illness because their immune systems are fragile.
E Coli O145, HUS and AKI
Over 10% of those diagnosed with such E coli infection can develop a potentially life-threatening complication known as haemolytic-uraemic syndrome (HUS). It usually does not cause HUS and follows this path:
From Tarr, 2005
Symptoms of HUS include fever, abdominal pain, tiredness, decreased frequency of urination, small unexplained bruises or bleeding.
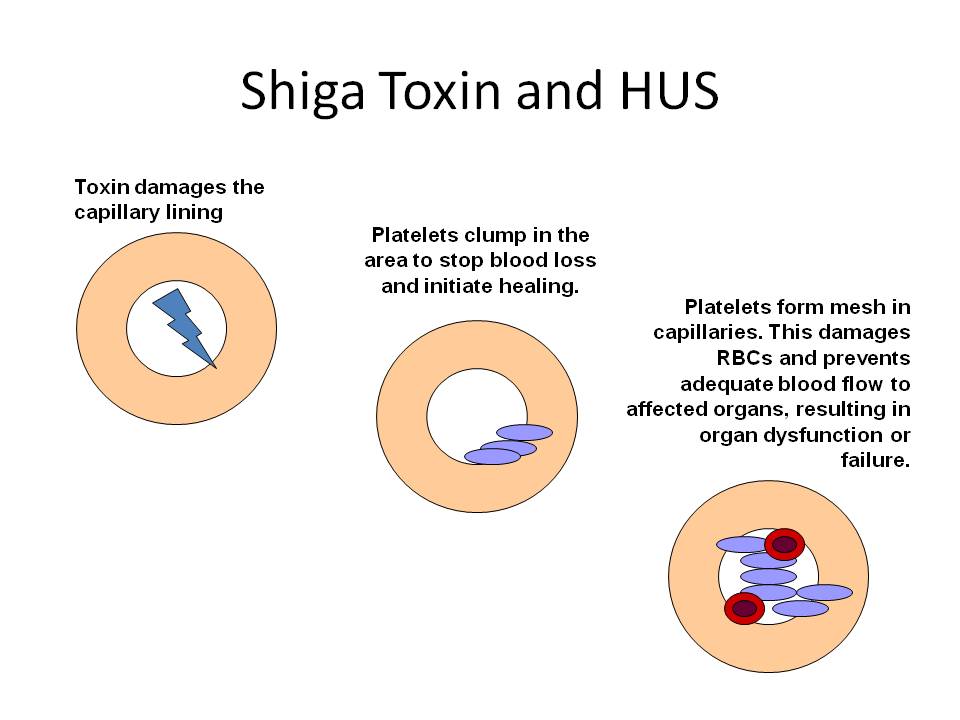
This is because and E Coli O145 (and other subgroups) can produce a Shiga toxin that can cause blood clots almost anywhere in the body (including the kidneys), and later (conversely) bleeding. This is how:
What is haemolytic-uraemic syndrome (HUS)?
It is a syndrome where there is clotting (and later bleeding) in small blood vessels all over the body. When it affects the kidneys, it shows itself as a triad of:
- Anaemia – microangiopathic haemolytic type (called a ‘MAHA’)
- Low platelets – thrombocytopenia
- Acute kidney injury (AKI).

Clinical features of HUS. Other bacteria (e.g. E Coli O157 and Shigella) cause produce STECs as well as shown in the diagram.
People who experience HUS symptoms should immediately seek emergency medical care. This will almost always mean hospital admission, because HUS can cause severe complications such as AKI, hypertension, strokes and other neurological problems.
Patients with AKI may require acute dialysis, and other special treatments including a very expensive drug called Eculizumab (for aHUS only).
HUS isn’t contagious. You cannot get HUS from person-to-person contact. But you can get E Coli from person-to-person contact and that can lead to HUS.
Causes of HUS
E Coli O145 is not the only cause of HUS. Here are the causes.
Primary (10%)
Atypical HUS (aHUS). Can occur in both adults and children due to abnormalities in the alternative complement regulatory pathway. Genetic mutations cluster in families. Some patients get recurrent episodes.
Secondary (90%)
- Diarrhoea-associated HUS (D+ HUS). Most common in children and usually caused by Shiga toxin-producing Escherichia colis (STEC; including o157 and 0145 subgroups) and other bacteria (Shigella, Salmonella, Camplyobacter)
- Malignancy
- HIV infection
- Solid organ and stem cell transplants
- Other autoimmune disorders
- Certain medication – e.g. ciclosporin/tacrolimus, chemotherapy agents, quinine, oral contraceptive pill.
Note. Post-partum HUS can occur upto 6 months after delivery
Summary
We have described the current E Coli O145 outbreak in the UK – and how it may cause HUS and AKI. We hope it has been helpful.
Other resources
Haemolytic uraemic syndrome (HUS)
Haemolytic uraemic syndrome review articles: Corrigan, 2001; Sheerin, 2019; Kuter, 2024
Argentina has the highest rate of HUS worldwide, with 70% of the cases associated with STEC infections: Carbonari, 2022
Last Reviewed on 14 June 2024
