History of haemodialysis
In this article we will describe the history of haemodialysis, a procedure where a dialysis machine and is used to filter blood before it is returned to the body.
History (upto 1914)
Scottish chemist Thomas Graham, known as the ‘father of dialysis’, first described dialysis in 1854. He used osmosis (the movement of water from an area of high concentration to an area of low concentration) to separate dissolved substances and remove water through semi-permeable membranes. Graham did not apply this concept to medicine straight away.
Instead, Graham was working as a chemist in Glasgow University at around the same time as physician Richard Bright was describing the clinical features and diagnosis of renal failure in Edinburgh.
He noticed that crystalloids (fluid made up of mineral salts dissolved in water) were able to diffuse through vegetable parchment coated with albumin (which acted as a semi-permeable membrane). He called this ‘dialysis’. Using this method he was able to extract urea from urine. Graham prepared a bell-shaped vessel shown below:
The wide open end of the bell was covered by a membrane created from an ox-bladder. He filled the bell-shaped vessel with urine and suspended it inside a larger container, filled with distilled water. After several hours, the bell-shaped vessel was removed. Then, the larger container was heated so that the fluid inside boiled to dryness.
Graham showed that the residue in the larger container consisted mainly of sodium chloride and urea, the principal components of urine. This proved that urea had passed through the membrane.
Graham termed this process dialysis and proposed, together with Richard Bright, that this would form the basis of a treatment for renal failure. They predicted that it would take around 60 years to develop the process sufficiently to be used in patients.
In 1855, German physiologist Adolf Fick published a quantitative description (a detailed account including the measurements – how much/many/often) of the diffusion process. Through their observations, Graham and Fick discovered the underlying principles of dialysis.
But their theories were not turned into practice until Albert Einstein defined diffusion laws thermodynamically as related to molecular motion. In so doing, he established a solid scientific basis for dialysis.
Aside from being the first to describe the process of separating substances with a semi-permeable membrane, in 1861 Thomas Graham also was the first to separate colloids and crystalloids using a parchment membrane. Graham realized that, for successful treatment of renal failure, toxins which accumulate in renal failure would have to be removed.
In order to do this, it would be necessary to understand the production rate of these toxins in the patient and the rate at which they can cross the membrane, so he made many measurements of rates of transfer across the membrane for different substances.
The science of dialysis being the adequate course of treatment depends on being able to understand renal failure, uraemic toxicity, and membrane function. In 1884, the British physiologist, John Berry Haycraft, first discovered hirudin, an anticoagulant(substance which stops blood from clotting), from leeches. His involvement and the history of anticoagulation has been reviewed by Mannucci in 2001.
The development of what eventually became a functional haemodialyser was the combined effort of several types of membrane, each an improvement on the last. Collodion membranes provided the first low flux dialysers.
Fick (1855) was perhaps the first to use collodion membranes to selectively separate small molecular weight solutes (MW < 5000) from blood through the process of diffusion (Eggerth, 1921). This was shortly followed by the preparation of collodion tubes and the manufacturing process to control pore size and water permeability (Ferry, 1936).
History (1914-1945)
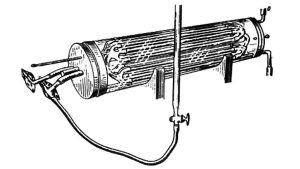
While significant research with artificial membranes, was conducted between 1880 and 1913, it was not until 1914 that John Abel, Leonard Rowntree, and BB Turner created the first artificial kidney, at the Johns Hopkins University School of Medicine. They used cellulose trinitrate (colloidin) tubes held in a glass ‘jacket’. The jacket was filled with saline or artificial serum; with an attached burette containing a solution made of hirudin.
Although this device was revolutionary it was never used on humans. That same year (1914), Hess and McGuigan recommended high blood flows to avoid clotting or need for anticoagulation. In 1916, Jay McLean, a second-year medical student, also at the Johns Hopkins University, was working under the guidance of William Henry Howell investigating pro-coagulant preparations.
During his investigations, he isolated a fat-soluble phosphatide anti-coagulant in canine liver tissue. It was Howell in 1918 who coined the term heparin for this type of fat-soluble anticoagulant in 1918. This was an important discovery in the history of nephrology.
In 1923, Heinrich Necheles in Hamburg, develops the first ‘sandwich’ artificial kidney using a biological membrane consisting of calves’ peritoneal membrane and dialysed dogs. In 1924, Georg Haas (1886-1971) performed the first human haemodialysis in a uraemic patient, at the University of Giessen (near Frankfurt) (Hass, 1925; Benedum, 1979).
He used a tubular device made of collodion, cannulated the radial and carotid arteries and the portal vein; and hirudin for anticoagulation. Later that year he added a blood pump. The dialysis lasted only 15 minutes, and no complications were observed or reported.
Stewart Cameron (2000) has emphasised the pivotal role of William Thalhimer (1886-1961), a non-clinical haematologist, in the history of haemodialysis, which has received little or no attention from historians of nephrology. Thalhimer had graduated from Johns Hopkins Hospital in 1908, where he was a pupil of Abel amongst others.
One of Thalhimer’s main interests at this time was blood transfusion, for which he employed heparin as an anticoagulant. He was intrigued also by the idea of exchange transfusion and its therapeutic potential.
In Chicago, in 1937, Thalhimer, used heparin for the first time, to allow exchange transfusion for alleviation of uraemia in nephrectomised dogs, using the first flat hemodialysis membrane made of cellophane. He then went on to construct an ‘artificial kidney’ with cellulose tubing 2 cm wide and 30 cm long, and an Abel‐type kidney to dialyse dogs, using heparin as an anticoagulant (Thalhimer, 1938). The dialyses lasted 3–5 h, and up to 1.5 g of urea could be removed.
Thalhimer’s vital contribution to the evolution of haemodialysis was the realisation that commercially available cellophane tubing could be used for in vivo dialysis. In 1940, heparin was used for the first time in human patients by the surgeon Gordon Murray of Toronto. Murray made further important contribution to the history of HD in 1946 (see below) and in transplantation in (see Transplantation chapter)
Born in Leiden, Netherlands, Willem Kolff (1911-2009, age 97 years) studied medicine in his hometown at Leiden University, and continued as a resident in internal medicine at Groningen University. One of his first patients there was a 22-year old man who was slowly dying of renal failure.
This prompted Kolff to perform research on artificial renal function replacement. Also during his residency, Kolff organized the first blood bank in Europe (in 1940). During World War II, he was based in Kampen, where he was active in the resistance against the German occupation
In 1940, while taking care of casualties after the German invasion of the Netherlands, his interest in acute renal failure further increased. And, in 1943, he and Hendrik Berk introduced the rotating drum hemodialysis system (Kolff, 1944). This used cellophane membranes and an immersion bath and the first recovery of an acute renal failure patient treated with haemodialysis was reported.
Working under Nazi scrutiny in the occupied Netherlands, he constructed the first machine out of common items, including a washing machine, orange juice cans and sausage skins
Early results were of limited success (the first 16 patients died). Then, on 11th September 1945, a 67-year-old woman, Sofia Schafstadt, a Nazi collaborator, was admitted to the Kampen Hospital suffering from acute cholecystitis with jaundice and acute renal failure with anuria, which it was considered had been caused by treatment with a sulphonamide.
She went into a coma, and Kolff and Berk connected her to the dialyser. After 11 hours’ dialysis, she regained consciousness and her health improved dramatically. Normal diuresis started within a few days and she made a good recovery — the first patient whose life had been saved by renal dialysis. She died some six years later from an unrelated cause.
This was the beginning of what was to become an important clinical reality: artificial renal substitution therapy. By the end of World War II, Kolff had constructed five of his dialysers, which he donated to hospitals around the world before moving to the United States to continue his research.
History (after 1945)
Gordon Murray, a surgeon in Toronto unaware of Kolff’s work, built a machine with which he did the first successful haemodialysis in North America, in December 1946. Although it was successful, his machine never came to anything for reasons given in an excellent 1999 article by Mckellar entitled, “Gordon Murray and the artificial kidney in Canada”.
In Sept 1947, Russell Palmer, in Toronto, carried out a successful HD, using the Kolff dialyser. In 1962, Palmer went on to design the first (soft) silicone PD catheter (made by Wayne Quinton). This was the first catheter that could be left in the abdomen permanently, providing continuous access to the peritoneum for the first time.
During the 1940s and 50s, there were significant improvements in dialyser and equipment design. Nils Alwall, at the University of Lund, Sweden, developed a new system with a vertical stationary drum kidney and circulating dialysate around the membrane (Alwall, 1947).
He was also responsible for applying hydrostatic pressure to achieve ultrafiltration, and pioneering the renal biopsy. It appears that Kolff, Murray and Alwall developed artificial kidneys at about the same time, unaware of each others’ work, partly due to the time period (WWII) when the research happened.
Alwalls contribution to nephrology didnt stop there. Stanley Shaldon (2003) has emphasised the role of Alwall in developing the AV shunt. The original idea of a bypass to maintain the patency of indwelling arterial and venous catheters was developed by Nils Alwall in 1948 and published in 1949 (Alwall and Bergsten, 1949).
In his first animal experiments in rabbits, the carotid artery and jugular vein were cannulated with siliconised glass tubes and patency was maintained with a curved siliconised glass capillary bypass. Following the success of the animal work, Alwall started treating patients with end stage renal disease (Alwall and Norvitt, 1949). However, because of local infection and clotting he abandoned the technique in 1949.
The high rate of death in military casualties who developed AKI had been noted in the WWII; and was seen again in the early part of the Korean War, when it was reported that 80-90% of soldiers with ARF died.
Because of this a specialist Renal Centre was established under the auspices of the US Army Surgical Research Team at the 11th evacuation Hospital of the 8th Army. Dr Paul Teschan arrived from the Walter Reed Army Medical Centre in Washington DC to lead this group in 1952, and soon after an artificial kidney arrived from Washington (Teschan, 1955).
In May 1954, the first ever symposium on the artificial kidney, occurred in Rapallo, Italy. Fogazzi (2003) described this symposium, in an article that is a good summary of the early years of haemodialysis.
Kolff in turn developed the coil dialyser using a tubular membrane wrapped around a solid core for use with a single pass dialysis fluid delivery system (Kolff, 1956). This was followed by the twin dialyser with twin blood pathways, the first disposable haemodialyser.
In 1960, Kiil developed the plate dialyser that could be reassembled (Kiil, 1960). The system consisted of multiple polypropylene boards supporting flat cellulosic membranes. This parallel flow kidney could be used without a blood pump due to its low resistance.
A new phase in clinical hemodialysis started with the introduction of the Quinton and Scribner AV shunt in March 1960. They further developed the work of Alwall in 1948, and designed silastic tubes fitted with Teflon tips, placing them in the radial artery and cephalic vein at the wrist (or the posterior tibial artery and saphenous vein) – creating an AV shunt.
The two tubes ended in expanded couplings to facilitate connection. This shunt provided for the first time continuous circulation of the blood when the patient was not attached to the machine, effectively eliminating clotting and provided ready access for repeated long-term haemodialysis, opening the door to chronic renal replacement therapy.
The next significant advance in vascular access occurred in the 1966 when Cimino, Brescia and Appel first described their native arterio-venous fistula (AVF) for chronic vascular access. These fistulas are generally created by an end-to-side vein-to-artery anastomosis. A mature native AVF is the safest and longest lasting vascular access for haemodialysis.
History of dialysis in the UK (c1950–1980)
The first maintenance haemodialysis unit in the UK was opened by Stanley Shaldon at the Royal Free Hospital in 1961. This was followed by David Kerr at Newcastle in 1963 and Hugh de Wardener at the Charing Cross Hospital in April 1964. Stanley Shaldon also launched the first home HD programme in 1964.
On 26 February 2008, there was a fascinating Witness Seminar on the development of dialysis in the UK (1950-80), held at the Wellcome Trust Centre for the History of Medicine at UCL, London (Crowther, 2009). The transcript of this meeting is well worth reading.
In the last four decades, the major developments have been related to improvements in membrane biocompatibility and dialyser design, volumetric control, sophisticated monitoring systems that provide online clearances, isothermal dialysis, high flux membranes and convective modalities such as haemofiltration and haemodiafiltration.
Summary
We have described the history of haemodialysis. We hope you have found it interesting.
Etymology
Haemo-
Via Old French hemo- , from Latin haemo-, from Greek haimo- , from haima = blood
-dialysis
1580-90. Via Latin, from Greek dialysis = ‘dissolution, separation’ (of the disbanding of troops, a divorce etc), from dialyein = ‘dissolve, separate’, from διά (diá, ‘inter’ ‘through’) and λύειν (lýein, ‘loosen’). Used originally in logic and grammar. First used in a chemistry sense in 1861, and in medicine in 1914
Not what you were looking for? See our other articles on haemodialysis:
Last Reviewed on 10 April 2024
