How to examine the heart and cardiovascular system (CVS)
Summary (‘PINHAT-CsAsT’)
- P – Pre-observation
- I – Introduction – start well
- N – Nails
- H – Handshake and hand – radial pulse, rate, rhythm, character (collapsing?)
Note. Signs of endocarditis can be apparent on the handshake (nails, palms and pulps of fingers for Janeway lesions/Oslers nodes etc)
- A – Arm (BP) – do NOT forget the BP
- T – The Neck (JVP)
- Cs
- Chest front – inspect, palpate, auscultate: 4 areas; roll left (MS/MR), sit forwards + expiration (AS). Listen carefully
- Chest back – inspect, palpate (sacral oedema), auscultate (basal crackles)
- As
- Abdomen (liver)
- Ankles (oedema) – ask to do pulses
- T – “Thankyou”
So. How to examine the heart and cardiovascular system (CVS) ..
Pre-observation
Observation is 90% of medicine. Antennae up. Observe. You start the examination before the introduction by looking for these things as they walk towards you, or you to them:
- Shortness of breath (SOB) – Congestive cardiac failure (CCF; what about other causes of fluid overload)?
- Ankle swelling – CCF (ditto)?
- JVP – if you can see it sitting at 90 deg or standing, it’s pathological
- Chest pain (pleuritic) – getting slowly out of chair, or holding chest.
What are they reading? Why?
Introduction
Shake the patient’s hand. This diagnostic handshake is part of examination as well as a greeting. Introduce yourself, confirm the patient’s name and age (date of birth takes too long). Explain what you are going to do.
“My name is John/Jane, and you are Mr X. Is that right? And how old are you sir/madam?”
“Thanks. I’m going to examine your heart now, is that OK?”
Then proceed to wash your hands. Adjust the bed to a 45° angle. Start.
General inspection (especially breathing)
Begin the examination by inspecting the patient from the end of the bed. The patient must be exposed (i.e. naked) from the waist up. Offer a sheet or towel to maintain their dignity, and inform women that they may keep their bra on. Expose their legs as well, as there may be some obvious oedema or venous ulceration.
Look (actively)
Look out for the following signs which will give you a good indication of the state of the patient at rest.
- SOB – this can be due to several cardiac pathologies ranging from CHF to pericarditis
- Cyanosis (central especially) – suggests low tissue oxygen saturation. Not very reliable. Central cardiac causes are usually congenital (usually R-to-L cardiac shunting)
- Pallor – suggests anaemia or reduced perfusion, although it may just be the natural complexion of the patient. Again not reliable. No use in non-Caucasian people.
Environs
Look for paraphernalia around the bedside, looking for clues such as oxygen and ECG leads. Patients with angina may have a GTN spray.
Also look for more subtle signs which may give clues to the patient’s pathology. E.g. a patient with CCF may be using a large number of pillows, fluid restricted and fitted with a catheter to monitor urine output.
Hands (especially radial pulse)
Fingers and nails
Inspection of the hands should be done in an intentional and noticeable way. Warm well perfused hands are a good sign. They should be similar colour. Look at the nails carefully for clubbing, which could be a sign of congenital cyanotic heart disease, infective endocarditis or atrial myxoma. Inspect the hand for other stigmata of endocarditis including:
- Splinter haemorrhages – tiny blood spots or splinters that occur under the nails due to microhaemorrhages. Causes include infective endocarditis, vasculitis, psoriatic nail disease, and trauma. They may be a carpenter.
 Splinter haemorrhages
Splinter haemorrhages
- Janeway lesions – painless macular lesions caused by septic emboli, only present on the palms

- Osler’s nodes – painful raised lesions usually on the fingers

Oslers node
Note. Who were Janeway and Osler? They may ask. No, not that Janeway (Star Trek one).
- Examine the fingers – long fingers (arachnodactyly) can be a sign of Marfan’s syndrome, a cause of aortic dissection. Inspect the joints and palm for xanthomas (yellow cholesterol-rich deposits), indicative of familial hypercholesterolaemia.
Capillary refill time – you can assess this next by applying pressure to the distal phalanx of the patient’s index finger for five seconds. The finger should turn pale but revert back to its normal colour within less than two seconds. Poor perfusion is a sign of shock. Another unreliable sign though. You won’t fail if you forget!
[Top Tip. When assessing the palm for pallor, a good tip is to compare the patients palm to your own. Temperature can be assessed by placing the dorsal aspect of your hand on theirs and comparing].
Radial pulse (rate and rhythm)
Palpate the right radial pulse at the wrist to assess rate and rhythm. An irregularly irregular rhythm is usually due to atrial fibrillation or ectopic beats. Learn the rarer causes.
When assessing rate, measure for 15 seconds and multiply by 4.
If you have time, briefly palpate the left radial pulse to compare and check for radio-radial delay, which could be a sign of aortic coarctation or aortic dissection. Offer to check for radio-femoral delay, which will also present in these conditions.
Collapsing pulse
Put your hand all the way around the wrist with the fingers touching the radial artery. Lift the patient’s arm up briskly (but gently) above the level of their heart and hold it. Palpate for a collapsing pulse (‘waterhammer’) pulse, a classic sign of aortic regurgitation (AR). It feels like a woodpecker on the inside of the wrist trying to tap its way out. Or a budgerigar.
 How to examine for a collapsing pulse
How to examine for a collapsing pulse
Brachial pulse (character)
MyHSN prefers to use the brachial to assess character rather than the ‘classical’ way of doing it (carotid).
Assessing the character of the pulse reliably requires a lot of experience. It can be described as normal, sharply-rising and falling (AR), thready (circulatory shock), or slowly-rising and falling (aortic stenosis, AS).
If you use the carotid pulse, the character of the waveform should be considered. A visible carotid pulse in the neck (Corrigan’s sign) is indicative of aortic regurgitation.
Arm (especially BP)
Blood pressure = equal most important sign of cardiac disease (with JVP)
Check the patient’s blood pressure. Ideally you would want to do this in both arms, as aortic dissection can present with a difference in blood pressure; and also when patient is both sitting and standing, as a difference would be found in postural (orthostatic) hypotension. There usually isn’t time. Either way ..
[Top Tip. Do NOT forget the BP. Full stop. Why? It tells you whether the heart is pumping effectively. Low BP is an ominous sign. A low BP with wide pulse pressure (say 90/70) can indicate AS. A high BP with wide pulse pressure (210/90) can indicate AR].
Face (especially eyes)
Eyes
Inspect the eyes for pallor (anaemia), corneal arcus and xanthelasma (dyslipidaemia). The eyes may also appear sunken in a dehydrated patient (unreliable). Periorbital oedema can occur in CCF but more usually renal disease (e.g. nephrotic syndrome).
Check the cheeks for a malar flush, a sign of mitral stenosis (or could be lupus!).
“Please open your mouth”
Mouth
Inspect the tongue and palate. Central cyanosis can be observed on the lips or on the underside of the tongue. Check the mouth for dental hygiene, as poor hygiene is a risk factor for infective endocarditis.
Macroglossia can be sign of amyloid, and a high arched palate can occur in Marfan’s syndrome.
Neck (especially JVP)
“I’m going to feel your neck, please turn your head to the left”
JVP = equal most important sign of cardiac disease (with BP)
Ask the patient to turn their head to the left and observe their jugular venous pressure (JVP). In healthy patients, this should be no greater than 4 cm, i.e. not seen or just visible. This is measured as the vertical height from the angle of Louis (sternal angle) to the highest visible point of the JVP. If the JVP cannot be observed, pressure can be applied to the liver to elicit a hepatojugular reflux.
When assessing the JVP it is important that the patient does not turn their head completely to the left nor tense their neck muscles. This can obscure visibility of the vein.
[Top Tip. The JVP can be distinguished from the carotid pulse by its double pulsation, and not being palpable (unlike carotids). You should know all the causes (not just cardiac) of a raised JVP. CCF, and all causes of fluid overload, are the commonest].
Chest – front (praecordium)
(Look)
Inspection
Inspect the praecordium (chest area over the heart) for anterior scars, chest wall deformities (e.g. pectus carinatum/excavatum) or visible pulsations. Common scars include:
- Midline sternotomy scar – midline of the thorax. Can be due to a previous coronary artery bypass graft, valve replacement or congenital correction
- Pacemaker scar – may be under the L clavicle (or hidden in axilla). Palpate to check it is a pacemaker
- Mitral valvotomy scar – lift L breast if necessary
- Axillary thoracotomy scar – 5th intercostal space in the anterior axillary line. Commonly due to a previous chest drain. This is best assessed when inspecting the back
- Posterolateral thoracotomy scar – located at the lateral and posterior intercostal space inferior to the tip of the scapula. Commonly due to a lobectomy or pneumonectomy. This is also best assessed when inspecting the back.
 Common chest scars
Common chest scars
Palpation
Palpate for the apex beat. This is found in the left 4th or 5th intercostal space in the midclavicular line. A displaced and sustained apex is caused by left ventricular hypertrophy. Palpate the areas of the four heart valves for thrills. These are palpable murmurs, which feel like soft vibrations. If present, they indicates a significant murmur. Their presence or absence is unreliable as a sign. The location of each valve is as follows:
- Mitral area – 5th intercostal space, midclavicular line
- Tricuspid area – left 5th costo-sternal border
- Pulmonary area – left upper sternal border at the 2nd intercostal space
- Aortic area – right upper sternal border at the 2nd intercostal space.

Four cardiac areas. But heart murmurs from those valves are not necessarily maximally heard there – see diagram below
It is good practise to localise the apex beat after having palpated it. This is done by keeping your right hand on the area of the apex beat and using your left hand alone to count the ribs from the angle of Louis.
Finish palpation by checking for a left parasternal heave (right ventricular hypertrophy).
“I’m going to listen to your heart, please lean forward”
Auscultation
Listen in the four areas using the landmarks above, with the diaphragm of the stethoscope (used to detect high-frequency murmurs). Be sure to palpate the carotid pulse whilst doing so in order to time any audible murmurs. Listen for the 1st and 2nd heart sounds and for any additional abnormalities. If you hear a murmur, determine if it is systolic or diastolic by timing it with the carotid pulse.
Performing the following manoeuvres can help accentuate the commoner (left-sided) heart murmurs. Auscultation of these murmurs is best performed on end expiration. This augments left sided murmurs. Inspiration augments the rarer right sided murmurs.
- Mid-diastolic murmur (due to mitral stenosis, MS) – maximal in mitral area. Can be accentuated by asking the patient to lie on their left side. Auscultate over the mitral area using the bell of the stethoscope. “Please roll on your left side”
- Pansystolic murmur (mitral regurgitation, MR) – mitral area, may radiate to the axilla. Therefore, whilst the patient is still lying on left side, auscultate for the murmur in the mitral area, and the axilla. Use the diaphragm again
- Early diastolic murmur (aortic regurgitation, AR) – tricuspid area. Accentuated by asking the patient to sit forward, and breathe out in expiration (“please breath in, breathe out and hold your breath”). Auscultate at the left lower sternal edge (tricuspid), rather than in the aortic area.
- Ejection systolic murmur (aortic stenosis, AS) – usually maximal in aortic area but can be loud and heard everywhere. May radiate to the carotid arteries. Therefore, with the patient already sat up, finish by auscultating the carotid arteries. AS is very difficult to distinguish from aortic sclerosis (AScl).
Rarer murmurs
Tricuspid regurgitation (TR; sounds like MR but maximal in tricuspid area and increased on inspiration).
Congenital – Aortic septal defect, ventricular septal defect, coarctation of aorta, patent ductus arteriosus.
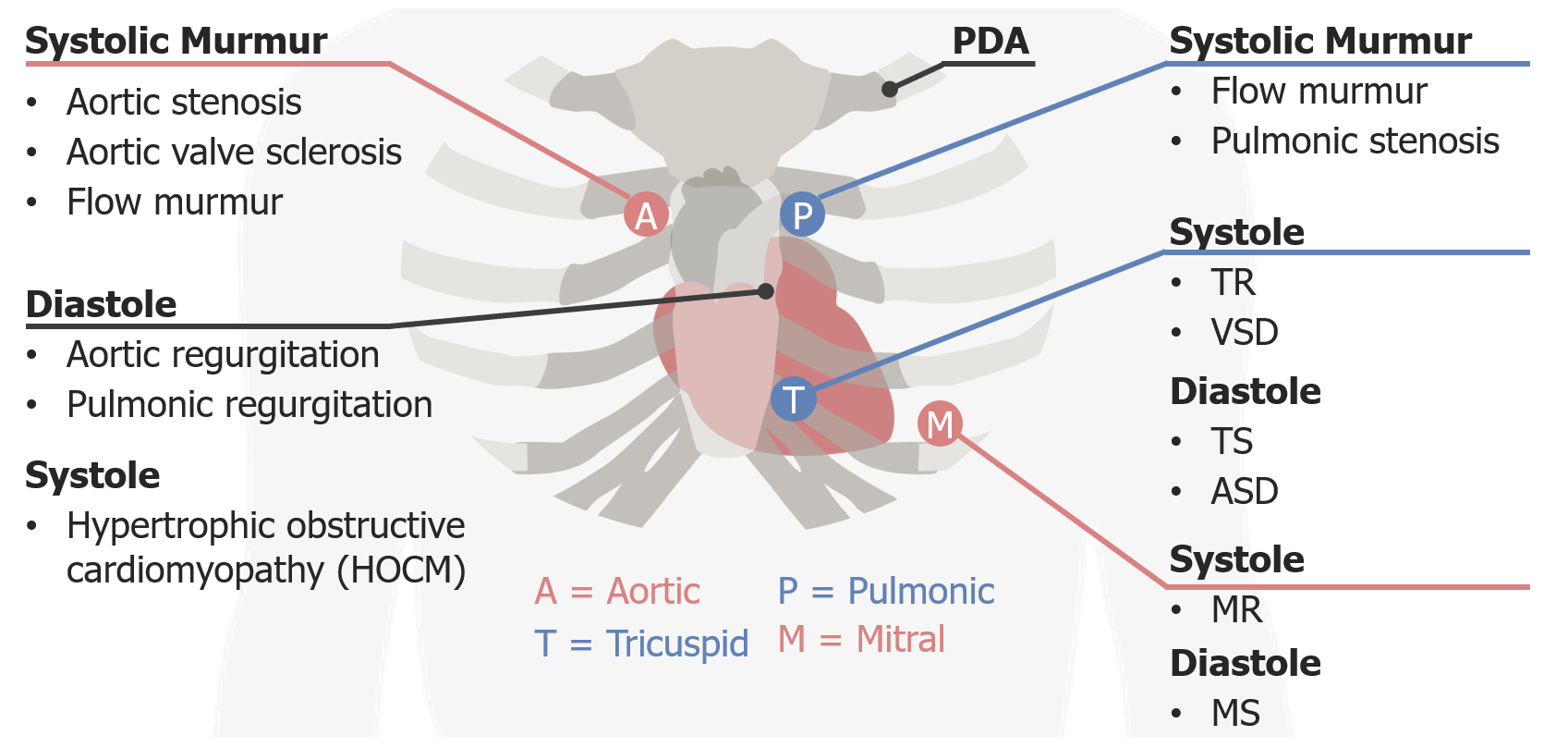
Type and location of murmurs
Auscultate and palpate carotid at same time
It is vital to palpate the carotid pulse whilst auscultating. This is how you determine if a murmur is systolic (in time with the pulse), or diastolic (immediately after the pulse).
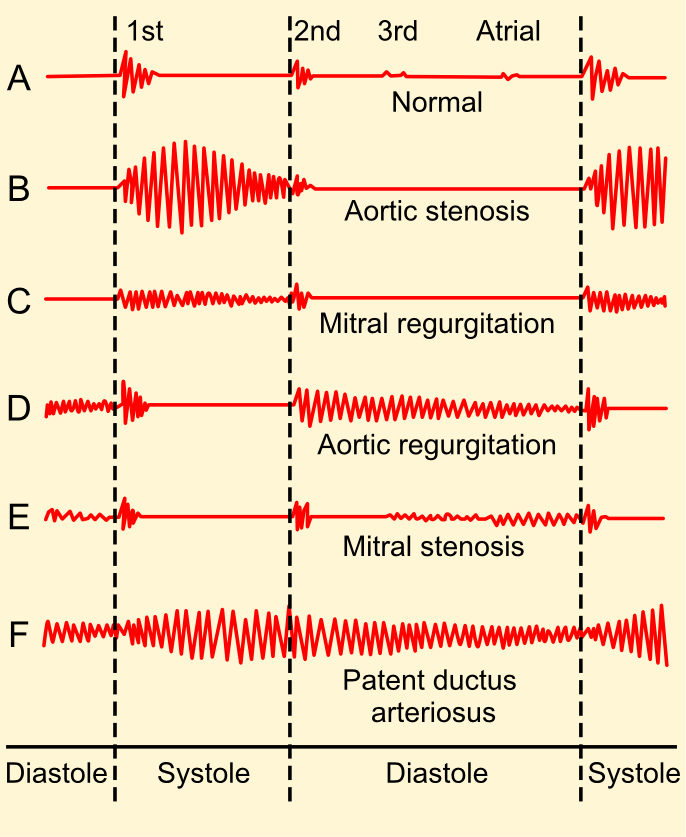 Timing of murmurs (related to heart sounds)
Timing of murmurs (related to heart sounds)
Carotid bruits
If you have time, after auscultating the neck for radiation of an ejection systolic murmur (e.g. AS), it is worth auscultating the carotids again – ideally with the bell of the stethoscope. This checks for carotid bruits, which are low-frequency, whooshing sounds due to turbulent blood flow. They are hard to distinguish from an AS/AScl murmur that has radiated to the neck. Older patients can have AS/AScl and carotid artery disease.
Chest – back
“Please stay sitting forward”
Complete inspection of the chest by examining the back for posterior and lateral scars. Palpate the sacrum for sacral oedema. Finally, auscultate the lung bases for crepitations (crackles). Sacral oedema and crackles are signs of right and left heart failure (RHF/LHF) respectively.
[Top Tip. It is good practise to move on to the back after auscultating the carotids, as the patient will already be sitting up. You do not want the patient to be constantly changing position as this is both uncomfortable and unnecessary.]
“I am going to lie you down now and examine your tummy”
Abdomen
Liver
Palpate the liver. A smooth enlarged liver can be a sign of RHF.
Abdominal aortic aneurysm (AAA)
Femoral pulses (and auscultate)
Femoral bruits are a sign of peripheral vascular disease, and/or a surrogate for renovascular disease.
[Top Tip. Ask to examine abdomen before you start. The examiner may say “not necessary ” (due to time). If so, move on to ankles].
Ankles
Check the patient’s ankles for pitting oedema, a sign of RHF (and all fluid overload states). Patients may also have PVD particularly if they have diabetes – so note any ulcers (and if present, offer to check for peripheral pulses).
If the patient has a midline sternotomy scar, this could be a result of a coronary artery bypass graft. Therefore check the knee, leg and ankle for scars due to saphenous vein harvesting.
[Top Tip. Again, at this point, you can ask to palpate the peripheral pulses, to show you can. Again, they will probably say “not necessary”].
Thankyou (completion)
“Thankyou very much sir/madam”
Complete the examination by offering to carry out a urine dipstick (to look for microscopic haematuria, which can occur in infective endocarditis). You could ask to interpret an ECG or carry out fundoscopy (‘silver-wiring’ and microaneurysms may be seen in hypertension and Roth’s spots may be seen in infective endocarditis). But there is a danger they may ask you to do it. This is why asking for a dipstick is safer.
Thank the patient and make sure they are respectable before drawing curtains are open.
We hope you now know how to examine the heart and cardiovascular system (CVS) better now.
Additional notes
- A pulsatile liver can be a sign of TR, and splenomegaly can occur in endocarditis
- If you hear femoral bruits, the patient may have an abdominal aortic aneurysm (feel and auscultate the epigastrium again) and/or renovascular disease
- Be nice to, and gentle with the patient – this is part of being a good doctor and scores you points in an exam.
Summary
We have described how to examine the heart and cardiovascular system (CVS). We hope it has been helpful.
Other resources
Medical diagnostic handshake
Dr James Gill, a friend of CKDEx, has a splendiferous You-tube channel with many great videos. here are some cardiac ones.
Last Reviewed on 2 July 2024
