Myths and facts about kidney stones
In this article, we will describe myths and facts about kidney stones.
Kidney stones (also called nephrolithiasis or urolithiasis) are very common, occuring in over 10% of the population, getting more common with age.
They affect approximately 1 in 5 males and 1 in 10 females by age 70 years. There is a high recurrence rate: 70-80% in males and 45-60% in females.
The kidneys, ureters and bladder are common sites where stones may be found. Common symptoms of having kidney stones are severe, unbearable pain, nausea and vomiting, blood in urine, etc.
However, some people who have had kidney stones, even for a long time, may not have any symptoms (silent stone), at all.
10 myths about kidney stones
1. Big Myth Number One – Everyone must drink 3-4 litres of water a day. And this helps to ‘flush out the kidneys’ which prevents kidney stones and UTIs
Many sources of information (mostly non-medical and of dubious reliability) dogmatically assert that humans 3-4 liters of water daily to stay well hydrated and thrive. CKDEx knows no evidence for this dogma.
Many people old people who drink a lot of water develop urgency, frequency and often urinary leakage. This can be dangerous as it can lead to falls (and their consequences including fractures and head injury).
Water requirements are based upon ambient temperature and activity level. If you are sedentary and in a cool environment, your water requirements are significantly less than when in the hot conditions.
Heeding your thirst is one of the best ways of maintaining good hydration status, in other words, drinking when thirsty and not otherwise.
2. Myth – All stones are painful
Not true. Yes, kidney stones are hard masses that form in the urinary tract and may cause pain, bleeding, or an infection or block of the flow of urine. But they are not always painful, especially when they first form.
Many stones cause no symptoms. And for some, the first signs of stones may be blood in the urine or minor back pain. In other cases, however, kidney stones can be excruciatingly painful and cause nausea and vomiting.
3. Myth – Larger stones are always more painful
Not true. Size is only one factor in how painful – and potentially dangerous – a kidney stone can be. The location of the stone is the other element to consider. A smaller stone in the wrong place can create a blockage that is incredibly painful and requires rapid admission to hospital via A&E.
Depending on the location of the stone, individuals may feel pain in their back or lower abdomen, or they may experience ‘renal colic’.
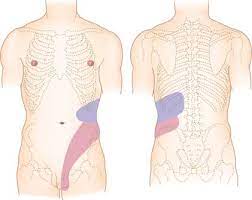
Site of renal colic, usually starting in the blue area.
This is excruciating, intermittent pain usually in the area between the ribs and hip on one side of the flank or back; it can spreads across the abdomen and often extends to the genital area. The pain tends to come in waves, gradually increasing to a peak intensity, then fading, over about 20 to 60 minutes.
4. Myth – Restriction of calcium in the diet helps to reduce urinary stone recurrence
75% of kidney stones are made of calcium oxalate. So many people believe that restriction of dietary calcium is a logical means of preventing a recurrence. This is not true.
But, in fact, several studies have shown that restriction of calcium in the diet actually increases the recurrence rate of kidney stones by increasing the oxalate absorption from the intestine.
So calcium should be consumed in moderation and should not be restricted.
5. Myth – Milk causes kidney stones because of its calcium content
Not true (see above). Calcium is your friend, so drink on. The fact is one-way kidney stones are actually caused is a lack of calcium.
6. Myth – Kidney stones always require urgent medical attention
Not true. Some kidney stones (mainly those that cause renal colic) require urgent medical treatment, but most do not need urgent attention.
For example, some individuals, including those with a family history or associated medical conditions such as Crohn disease or ulcerative colitis, are more likely to have chronic or repeating kidney stones. These people can develop strategies for safely managing pain and passing stones at home.
7. Myth – Kidney stones are more common in men
Not true. A few decades ago, men were far more likely to develop kidney stones. That’s no longer the case. Many more women are suffering from kidney stones today, and men and women are just about equally as likely to develop them.
Researchers believe there are many reasons for this shift, including people in the western world eating a more acidic diet today as well as an increase in the prevalence of obesity, diabetes and other risk factors.
8. Myth – If the pain goes away, you’ve passed your stone
Not true. Unfortunately, the relief that comes from subsiding pain does not necessarily mean the stone has passed. The level of pain can vary as the stone grows and moves.
Studies show that of the stones that pass themselves. In fact 95% will pass within four to six weeks.
However, if the pain does not subside after about a month, the potential of the stone passing itself is reduced, and you will need to see a kidney surgeon (urologist) to get it removed.
9. Myth – Extracorporeal Shock Wave Lithotripsy (ESWL) can be used to treat renal calculi of any size and form
Not true. ESWL – which uses sound energy to shatter stones – is used to treat only smaller calculi (less than 2 cm). If ESWL is used to fragment larger stones, then the fragments may block the ureter; or some of these fragments may remain in the kidney and lead to a recurrence. Also it is not ideal for very hard stones.
10. Myth – If you have one stone, it is unlikely you will get another
Not true. Kidney stones are a very common disease that occurs in over 10% of the population, with a recurrence rate of 70-80% in males and 45-60% in females.
10 facts about kidney stones
1. Fact – What are kidney stones?
Most waste chemicals are dissolved in the urine (hence the urine is clear). But chemicals sometimes form tiny crystals in the urine which clump together to form a small stone. They vary in size from a grain of sand to a golf ball. Surprisingly, not that much is known about them.
2. Fact – How are the kidneys linked to the bladder?
Urine travels from each kidney down a tube (the ureter) draining urine from the kidney into the bladder. It is then released from the body when you have a wee. The whole system is called the urinary tract.
The human bladder is small (300 ml, about the size of a Coke can) and most humans pass about 1500 mls of urine a day (if they drink 2 litres a day). Hence, they will pass urine about 5 times, i.e. 5 x 300 ml = 1500 ml. The more you drink, the more urine you will pass.
 Kidney stone stuck in right ureter (in a man)
Kidney stone stuck in right ureter (in a man)
3. Fact – Types of kidney stone
There are four main types of kidney stones:
1. Calcium – this is the most common type of kidney stone, which occurs in about 70-80% of cases. Calcium stones are usually composed of calcium oxalate, and less commonly, of calcium phosphate. Calcium oxalate stones are relatively hard and difficult to dissolve with medical management. Calcium phosphate stones are found in alkaline urine.
2. Struvite – struvite (magnesium ammonium phosphate) stones are less common (about 10-15%) and result from infections in the kidney. A struvite stone is more common in women and grows only in alkaline urine.
3. Urate – are not very common (about 5-10%) and are more likely to form when there is too much uric acid in the urine and urine is persistently acidic. Uric acid stones can form in people with gout, who eat a high animal protein diet, are dehydrated or have undergone chemotherapy. Urate stones are radiolucent. This means they are not detected by an x-ray of the abdomen.
4. Cysteine – are rare and occur in an inherited condition called cystinuria. Cystinuria is characterized by high levels of cysteine in the urine.
 Types and sizes of kidney stones
Types and sizes of kidney stones
Some can be very large and fill up most of the drainage areas of the kidney(s). These are called staghorn calculi (stones) like in this x-ray.
 Staghorn calculi (stones) in both kidneys on an x-ray
Staghorn calculi (stones) in both kidneys on an x-ray
4. Fact – Risk factors
You are more likely to form a kidney stone if your urine is concentrated. For example, if you exercise vigorously, or live in a hot climate, or work in a hot environment, you may lose more fluid as sweat and less as urine.
You are also more prone to develop kidney stones if you have:
- Repeated (recurrent) urine infections
- Repeated (recurrent) kidney infections
- An abnormal kidney – for example, with scars or cysts on it. One example is an inherited illness called Polycystic Kidney Disease (PCKD)
- A close relative has had a kidney stone.
5. Fact – Causes
Underlying causes are uncommon. In a small number of cases, a medical condition causes the kidney stone. Various rare diseases can lead to high levels of chemicals in the body, such as calcium, oxalate, uric acid and cysteine. If the level of these chemicals is high enough in the urine, they can form into stones.
- ‘Water’ tablets (diuretics) – especially ones called thiazide diuretics;
- Some chemotherapy for cancer;
- Some medicines used to treat HIV.
However, most people safely take these medicines without developing kidney stones. If you think that a medicine you are taking is the cause of your kidney stone, you should not stop taking the medicine but discuss it with your doctor.
6. Fact – Symptoms
“Kidney stones can exist without symptoms for years.”
For some people, a kidney stone may just stay in a kidney and cause no symptoms. Other kidney stones may travel out of your body in your urine without you knowing anything about it.
“Kidney stones occur most frequently in the kidney and ureter.”
So, if kidney stone symptoms do occur, they usually relate to the kidney or ureter, and include:
- Pain from a kidney. A stone that is stuck in a kidney may cause pain in the side of your tummy (loin) or back. This pain can vary intensity from a long-term dull ache to severe pain
- Renal colic:
- This is a severe pain which is caused by a stone passing into the tube (the ureter) draining urine from the kidney (as in the diagram above) and becoming stuck. The ureter squeezes the stone towards the bladder, which causes intense pain in the side of your tummy (loin) or back
- The pain caused by renal colic may last from a few minutes to a few hours. The pain comes in spasms and between these spasms there may be intervals of no pain or just a dull ache
- The pain may spread down into the lower abdomen or groin. You may sweat, feel sick or vomit because the pain can be very bad;
Note. If you get these symptoms, you need to go to your nearest Accident and Emergency department. If you are first assessed by a junior doctor, you then need to see a more senior one (consultant, or their deputy called a registrar), who has specialised in surgery (or better urology; these are surgeons who have specialised in surgery to the urinary tract).
- Blood in your urine. You may see blood in your urine (i.e. your urine turns red). This is caused by a stone rubbing against the inside of your kidney, ureter or bladder
- Urine infection. Urinary tract infections (UTIs) are more common in people with kidney stones. UTIs may cause a fever, pain on passing urine (dysuria) and a need to pass urine more often (frequency).
7. Fact – Investigation
- Blood test (called ‘U&Es’) – to check that the kidneys are working properly. Very few patients with kidney stones, get kidney failure (called chronic kidney disease (CKD) Stage 4 or 5) and go to need kidney dialysis or a transplant;
- Other blood tests – these may be needed to check the level of certain chemicals that may cause kidney stones (if the level is high). Examples include calcium and uric acid
- Urine tests – to check for infection tract infection (MSU) and for certain crystals
- X-rays or scans – if you have kidney stone symptoms, special x-rays or scans of the kidneys, ureters and bladder are likely to be necessary. Most have to be done in hospital
These tests may start with an abdominal x-ray (and perhaps an ultrasound). A special type of CT called a ‘CT-KUB’ (CT of kidney, ureter and bladder) may also be needed. These tests will detect a stone, find out exactly where it is, and guide the doctor to what they need to do about it.
8. Fact – Treatment (medical)
Most small kidney stones won’t require invasive treatment. You may be able to pass a small stone by drinking more water. Drinking as much as 3 litres a day will keep your urine dilute and may prevent stones from forming. Unless your doctor tells you otherwise, drink enough fluid to produce clear or nearly clear urine.
9. Fact – Treatment (surgical)
If your kidney stones are too big to be passed naturally, they are usually removed by surgery. There are various types.
For certain kidney stones – depending on size and location – your doctor may recommend a procedure called extracorporeal shock wave lithotripsy (ESWL). You are awake for this treatment.
ESWL uses sound waves to create strong vibrations (shock waves) that break the stones into tiny pieces that can be passed in your urine. In other words, they are removed without a cut to the tummy.
Other surgical techniques – like ureteroscopy and percutaneous nephrolithotomy (PCNL) – may also be necessary to remove the stone(s). They happen under general anaesthetic, where you are asleep.
10. Fact – Recurrence (and prevention)
As there is a high risk of recurrence (45-80%), increasing fluid intake, dietary restriction and periodic check ups are necessary for most patients.
If you have had more than one episode, you should be referred to a urologist (kidneys surgeon) and various tests need to be done including:
Analysis of passed stones – if you have passed and saved one or more stones, they should be analysed to determine the composition (e.g. calcium oxalate, urate etc)
Urine tests – a 24-hour urine collection: this involves saving all the urine you produce over a 24-hour period, which then gets analysed at the laboratory
Blood tests – blood tests for kidney function, calcium and urate levels.
Summary
We have described myths and facts about kidney stones. We hope it has been helpful.
Last Reviewed on 19 April 2024
