Renal bone disease and CKD
Keep track of your kidney data with PKB
Renal bone disease (RBD), fortunately, largely affects patients in the more advanced stages of CKD, i.e. CKD4-5. Up until then it does not usually need to be monitored. After then, in many patients, it should be monitored – using blood calcium, phosphate and parathyroid hormone (PTH) levels.
But. Why does CKD cause bone disease? What symptoms does RBD cause? How is it monitored? How is it treated? We will now address these and other questions.
Let’s start with the basics about renal bone disease.
1. What is renal bone disease?
Renal bone disease, also known as renal osteodystrophy, is a complication of Chronic Kidney Disease (CKD) which affects the bones, causing them to be weaker.
Click here to read about the different types of renal bone disease.
2. How common is renal bone disease?
It is common in the more advanced stages of CKD.
Renal bone disease is not normally a problem for patients with CKD1-2 and CKD3A.
However, 50-75% of patients with CKD3B-4, and 90% of those with CKD5 (on dialysis or with a kidney transplant), have some evidence of renal bone disease on blood tests.
3. What causes renal bone disease?
- Mineral imbalance
Renal bone disease is primarily caused by the mineral imbalance that occurs in the body due to reduced kidney function. The kidneys play a crucial role in maintaining proper levels of calcium and phosphate in the blood and bones.
- Decreased vitamin D levels
Kidneys help activate (strengthen) vitamin D, which is necessary for calcium absorption from the intestines. In CKD, this activation is impaired, leading to decreased levels of active vitamin D and subsequently reduced calcium absorption – lowering calcium levels in the blood.
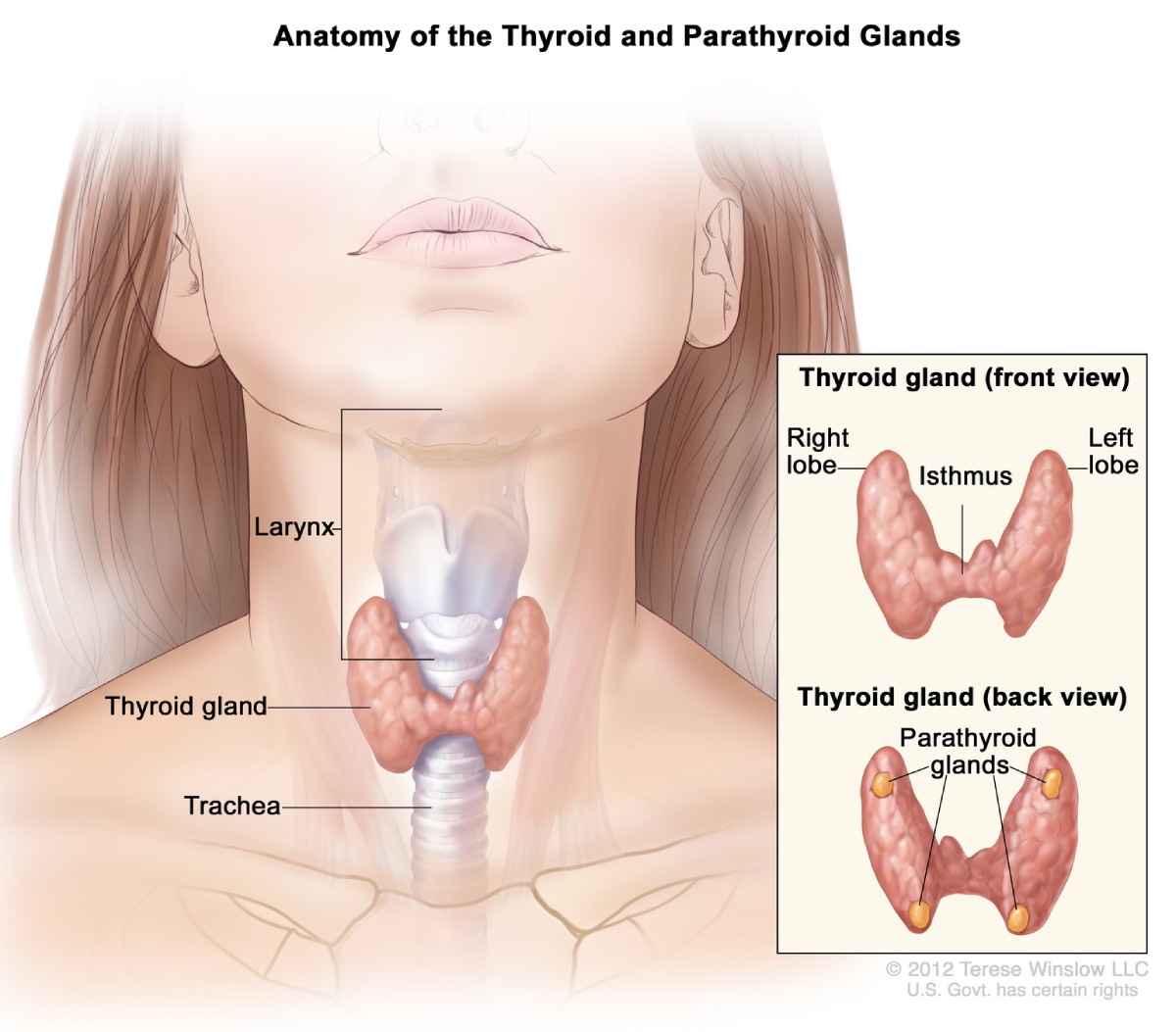
As a response to low calcium levels, the parathyroid glands (4 small glands on the back of the thyroid gland in the front of the neck) become overactive, leading to increased secretion of parathyroid hormone (PTH). This is called secondary hyperparathyroidism.
Growth of the parathyroid glands results in the release of calcium from the bones (in an attempt to raise calcium levels), causing bone pain and weakening. This can eventually lead to fractures.
- Increased phosphate levels.
Phosphate levels in the blood are increased as kidneys are less able to remove phosphate as kidney function worsens, and as a response to the low calcium levels.

4. What are the symptoms of renal bone disease?
- Bone pain. This often affects overall quality of life
- Fractures. This occurs due to bone mineral density loss (meaning the bones are weaker and so more susceptible to fractures).
5. How is renal bone disease diagnosed?
A diagnosis of renal bone disease is confirmed by a blood test.
The following characteristic pattern is seen:
- Low vitamin D levels
- Low calcium (<2.1mmol/L)
- High PTH
- High phosphate (>1.4mmol/L)
Note: Normal blood calcium is 2.2-2.6 mmol/L. In some patients with renal bone disease, after several years, the calcium can become high (over 2.7 mmol/L) rather than low. This will require a different approach (see below).
6. How is renal bone disease managed?
Managing renal bone disease requires a multidisciplinary approach involving nephrologists (hospital kidney specialist), specialist nurses and dietitians.
Treatment (in accordance with NICE guidelines) focuses on managing the underlying chronic kidney disease (CKD), controlling mineral imbalances and therefore preventing fractures.
Lifestyle – dietary changes can be made to help regulate calcium and phosphate levels. Click here for more information on nutrition and CKD.
Tablets – specific medications can be given to help correct mineral imbalances.
- “Phosphate binding” tablets (these reduce phosphate levels), e.g. calcium acetate
- Vitamin D supplements, e.g. alfacalcidol
- Other medications, e.g cinacalcet

Note: In the past, the use of aluminium-based tablets to control phosphate levels in CKD patients contributed to aluminium accumulation in the bones, causing bone disease. However, this has become less common with newer treatments.
Further treatment – In CKD5, dialysis also aids in the correction calcium and phosphate abnormalities.
Surgery – sometimes parathyroid surgeons are required to remove the parathyroid glands (parathyroidectomy) when treatment with tablets and diet (+/- dialysis) has not controlled renal bone disease sufficiently – and calcium levels are running high (over 2.7 mmol/L).
There are different approaches to a parathyroidectomy. In other words, different surgeons carry out slightly different operations. Whatever operation is done, it may be necessary to continue some of the renal bone diseases tablets you are taking. A few patients can come off all such tablets.
Summary
We have described renal bone disease and CKD. Yes, but largely in the later stages. We hope it has been useful.
Other resource
Function of kidney 6: vitamin D activation
Top tips for patients to prevent renal bone disease
There are things you can do to help:
- Blood tests. If you are in CKD4 or higher, have your blood calcium and phosphate measured at least every 3 months, and PTH every 6 months. Ask your doctor what the results show and whether you need any treatment
- Take medication. If you are prescribed tablets like calcium acetate and alfacalcidol, take them carefully.
Last Reviewed on 18 June 2024