Retroperitoneal fibrosis (RPF) – overview
Retroperitoneal fibrosis (RPF) is a rare condition in which there is fibrous tissue (scarring) in the retroperitoneal space, which is located behind the abdomen (tummy), in front of the spine.
Here is an overview of retroperitoneal fibrosis.
1. Definition
In retroperitoneal fibrosis the scar tissue in the retroperitoneum can compress (and block) nearby structures such as the ureters (tubes that carry urine from the kidneys to the bladder) and other abdominal organs. When it blocks the ureters it can cause AKI, CKD or AKI on CKD, and so is a (albeit rare) cause of obstructive nephropathy.
2. What is the retroperitoneum?
The retroperitoneum is the part of the body behind the abdominal cavity and in front of the back muscles and spine. This is where the main artery (aorta) and vein (vena cava) lie, taking blood to and from the lower half of the body. The tubes that drain urine from the kidney into the bladder (ureters) also run through this region.
RPF develops in this region surrounding the blood vessels and ureters – as shown in the following diagram.
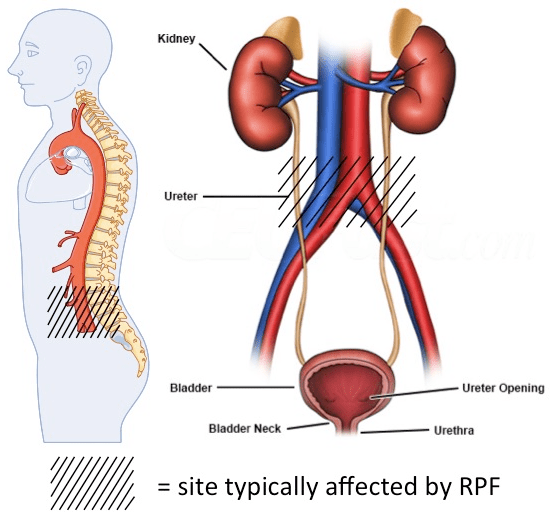
Areas commonly affected by RPF
3. How does it happen? Inflammation and scarring
Normally when there is a wound or an infection, the immune system identifies the affected area and it becomes inflamed. Next, scar tissue is laid down to ‘seal off’ a damaged area. Much later there is re-modeling and the fibrous scar tissue is reduced and original structures restored.
In RPF there is inappropriate deposition of fibrous scar-like tissue, indicating a problem with the normal control of the inflammation-scarring-healing process.
The excess fibrous material constricts and compresses normal structures. It can be seen on scans as extra tissue most often around the aorta.
4. Causes
The cause of retroperitoneal fibrosis is unknown in 70% of cases of RPF. When the cause is unknown, RPF is considered a chronic periaortitis, a presumed autoimmune large vessel vasculitis (inflammation of blood vessels).
In 30% of cases a cause is identified. Numerous drugs have been implicated in the development of RPF. Drugs such as methysergide (and other ergot alkaloids) are most commonly associated with this condition. Other medications that have been implicated include beta blockers, methyldopa, hydralazine, and analgesics.
The biological agents etanercept and infliximab have also been identified as secondary causes.
Malignancy (carcinoid, Hodgkin and non-Hodgkin lymphoma, sarcomas), infections (TB, histoplasmosis, actinomycosis), radiation therapy for testicular seminoma, colon, and pancreatic cancer, retroperitoneal hemorrhage and surgery, are all secondary causes of retroperitoneal fibrosis. Studies have demonstrated exposure to asbestos, and smoking may result in increased risk of RPF.
Association with IgG4-Related Disease
In some cases, retroperitoneal fibrosis is associated with ‘IgG4-related disease’, a systemic autoimmune condition that can affect various organs. IgG4 disease can be diagnosed with a blood test. If positive, treatment for a patient with RPF can be targeted to the underlying immune problem.
5. Who gets it?
Retroperitoneal fibrosis is a rare disease. It can affect individuals of any age but is more common in adults, aged 40-60 years. It is more common in men than women by a ratio of 2:1 to 3:1. The true incidence is unknown but is estimated to be 1 per 200,000 to 500,000 per year. This is a Japanese study of 49 patients with RPF.
6. Symptoms
The symptoms of RPF vary but include back or flank pain, abdominal pain, weight loss, and symptoms related to the compression of the ureters, leading to hydronephrosis (dilation of the kidneys). This can cause CKD, or AKI, or AKI on CKD – with the symptoms of those conditions.
7. Diagnosis
Diagnosis can be suggested by an ultrasound of the kidneys, but computed tomography (CT) or magnetic resonance imaging (MRI) gives more detail. Blood tests will be required to check kidney function and look for possible underlying causes.

CT scan showing RPF (arrowed) around the aorta and vena cava. There is hydronephrosis (blockage) of the ureters blocking the flow of urine from the kidneys.
A tissue sample (biopsy) may be required to confirm a diagnosis in some cases. If so it is usually done as a day-case procedure.
8. Treatment
The aims of treatment are:
- To slow down the inflammation and scarring process
- Protect kidney function
- Reduce pain
- Avoid complications.
Management of retroperitoneal fibrosis often involves relieving the obstruction caused by the fibrous tissue. Steroid tablets are commonly used to reduce inflammation, and in some cases, other immunosuppressive medication may be needed. Surgery may be necessary in severe cases.
If there is an underlying cause, this needs to be treated as well – e.g. radiotherapy and chemotherapy for lymphoma; or antibiotics for TB.
Surgical treatments
If a kidney is blocked it may be necessary to drain it with a tube placed straight into the kidney through the skin at the back (nephrostomy).

Nephrostomy
This is usually a temporary measure, and can be followed by using an internal stent in the ureter, connecting the kidney to the bladder. This is usually done in a minor operation under general anaesthetic (GA; where you are put to sleep under the care of an anaesthetist). A kidney surgeon (urologist) guides the stent into position using a ‘telescope’ inserted into the bladder. Stents need changing every few months as they are prone to silt up.
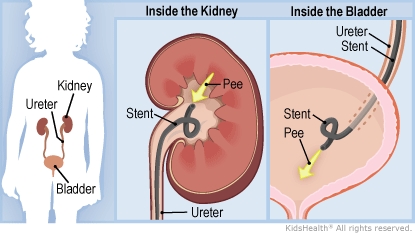
Ureteric stent
A long-term solution to ureteric obstruction is an operation called ureterolysis (surgical separation of the ureters from the fibrous tissue). This allows a patient to be stent–free and may provide the best relief of obstruction in selected cases. It is a big operation and may require several days in hospital and a number of weeks of recovery at home.
The treatment of RPF has been reviewed in this paper: Tanaka, 2020.
9. Prognosis (outlook)
The prognosis of RPF is variable. Often within a few days of initiating treatment the patient’s symptoms begin to improve. After several weeks, CT imaging may demonstrate significant improvement of the scar tissue. If medication is not effective, surgical treatment can protect the ureters.
However, the disease can recur, and long-term follow-up is often necessary.
10. Complications
If left untreated, retroperitoneal fibrosis can lead to serious complications such as AKI (requiring dialysis), or stage 5 CKD (kidney failure) due to prolonged obstruction of the ureters. Therefore prompt diagnosis and intervention are crucial to prevent irreversible damage.
Summary
We have described an overview of retroperitoneal fibrosis (RPF). We hope it has been helpful.
Other resource
Here is more information about retroperitoneal fibrosis.
Last Reviewed on 25 November 2023
