Should patients with renovascular disease have a renal angiogram/plasty and stent?
The short answer, in most cases, is no. We will now explain why
Renovascular disease (RVD) is a condition where there is narrowing or blockage of the renal (kidney) arteries, which supply blood to the kidneys. It leads to reduced blood flow to the kidneys, which in turn affects kidney function and raises blood pressure. It is a cause of CKD and AKI, and high blood pressure (that can be severe) mainly in older people, especially smokers.
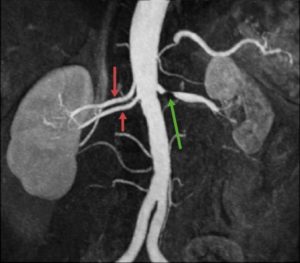
A renal angiogram – showing a stenosis (tightening) of the left renal artery and a ‘double artery’ on the right. Such variants are not unusual.
Even though it is a controversial area, most nephrologists (kidney specialists) rarely request a renal (kidney) angiogram and angioplasty/stent – either to investigate or treat patients with renal artery stenosis).
There are some exceptions. Most nephrologists would consider this investigation/treatment in these 5 groups of patients:
- Acute pulmonary oedema (or acute worsening of of heart failure) and high-grade RAS – sometimes called ‘flash pulmonary oedema’
- Progressive CKD in high-grade (>75%) RAS (bilateral or solitary kidney)
- AKI due to acute renal artery occlusion or high-grade RAS
- ACEi or ARB intolerance in high-grade RAS
- Kidney transplant with RAS (symptomatic or asymptomatic).
This is based on current international guidelines: KDIGO, 2022.
Summary
The balance of opinion is that renal angiogram/plasty +/- stent is not recommended for most patients with RVD. But it is a controversial area. And this question has recently been reviewed by Sarafedis, 2023 (with European Guidelines presented) and Theodorakopoulou, 2023. CKDEx would be interested in your view.
CKDEx has more information on what is a renal angiogram and angioplasty.
This article was reviewed by Dr Phil Kalra, Consultant Nephrologist, Salford Royal Hospital.
Last Reviewed on 3 March 2024
