Supportive care of CKD
Keep track of your kidney data with PKB
Key Points
- Supportive care means not having dialysis
- Dialysis does not suit everyone, especially frail elderly patients
- If you are on dialysis or with a failing transplant, you don’t have to continue with either
- Many symptoms can be controlled with tablets and injections
- Ask your kidney unit if they have a nurse that specialises in supportive care.
What is supportive care of CKD?
Supportive care means non-dialysis care – especially for those with advanced CKD, i.e. CKD4 and CKD5. It is also called palliative or conservative care, or medical management.
Dialysis is a hard life and does not benefit all patients. This is why some frail elderly patients prefer not to have the burden of dialysis.
Kidney doctors are also not sure whether dialysis works in this group. In other words, we do not know whether it prolongs life, or if its does, it could be by a little. Research is going on at present to answer this important question.
Also some patients who have been on dialysis prefer to stop. And some transplant patients prefer not to have dialysis or another transplant, if their transplant fails.
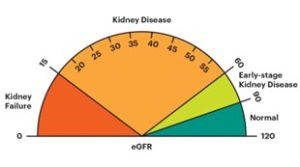
Different grades of CKD and symptoms
Doctors and nurses use a classification of severity of CKD (based on something called eGFR) to decide upon whether you need treatment. This also predicts whether you are likely to get CKD symptoms. Most do not get symptoms unless they are at the more serious end of the scale.
- CKD1+2 – risk factors for CKD – no CKD symptoms
- CKD3A+B – mild CKD – mild/no symptoms
- CKD4 – moderate CKD – some symptoms
- CKD5 – severe CKD (kidney failure) – significant symptoms.
CKD symptoms
If you do have symptoms of CKD, they may include (but are not limited to) the following:
- Itching
- Restless legs
- Nausea and loss of appetite (and lack of taste of food)
- Pain
- Feeling of deep cold
- Tiredness and fatigue
- Difficulty concentrating
- Leg cramps
- Shortness of breath and ankle swelling
- Depression/anxiety
- Poor sleeping
- Impotence or lack of sex drive.
Many of these symptoms are non-specific, i.e. can be caused by another disease.
Nonetheless, if you are not sure if symptoms are caused by CKD, it is still worth raising your symptoms with your kidney specialist doctor or nurse.
Symptom control in CKD4 and CKD5 is difficult. Having higher grades of CKD limits the use of medication (as drugs are not removed from the body by the kidneys). Doses may have to be adjusted – you can ask the kidney pharmacist to check you are on the right doses. Also, the treatment will vary, depending on whether you are: before dialysis (‘predialysis’); on dialysis (and which type); with a transplant; or having supportive care (not having dialysis).
If you choose supportive care, your kidney doctors and nurses will then focus on symptom control.
Symptom control
The following treatments may help. If you have tried these drugs with little effect, there are others. Ask your doctor or nurse to think again.
- Itching – see below
- Restless legs – Clonazepam
- Nausea and loss of appetite – small amounts high quality food, food supplements (ask to see dietitian)
- Pain – Gabapentin, Duloxetine
- Feeling of deep cold – no specific treatment
- Tiredness and fatigue – Erythropoeitin (EPO) and iron injections
- Difficulty concentrating – no specific treatment (but ask to see a psychologist)
- Leg cramps – Quinine sulphate
- Shortness of breath and ankle swelling – diuretics (Furosemide or Bumetanide), fluid restriction (less than 1.5 litres a day) or more dialysis
- Depression/anxiety – Duloxetine (also good for pain); and drugs called SSRIs, like Citalopram and Sertraline. And/or ask to see a psychologist
- Poor sleeping – Mirtazepine
- Impotence or lack of sex drive – EPO will help; also consider referral to Urology; and/or discuss with a psychologist.
Note. It is better to avoid Aspirin and similar drugs (called NSAIDs) for pain, as they can make the kidney function worse quite rapidly, especially if taken in high dosage for more than five days.
Itching
This is one of the most challenging symptoms to treat. Drug treatments have some effect but it is not huge. If you are on dialysis, Gabapentin can be a good choice, along with topical application of aqueous cream with 1% menthol (for its cooling effect).
But Gabapentin will build up in the bloodstream of patients who have chosen not to have dialysis. In such patients, very small doses – 50mg or 100mg alternate nights – are recommended (with early review for side effects, e.g. drowsiness and sedation). Capsaicin cream 0.025% QDS (4 times a day) is also useful.
A high calcium and phosphate level in the blood can make itching worse. Ask your doctor to check they are not abnormal, and correct them if they are. Having more dialysis may help itching but may be more work for you, or time on dialysis. So it’s hard to decide on that trade-off.
Referral to a skin specialist (dermatologist) may also help. Ask for that, if symptoms are not being controlled.
Supportive care and symptom control
If you are in CKD4 or CKD5, the question of dialysis (plus a transplant in some) will come up. You do not have to have dialysis. You do not have to have another transplant (and have dialysis again), if a transplant is failing. It is a hard life being on dialysis, and it may not suit many older frail patients – or make them live much longer. This partly as dialysis is not that effective, as it provides only about 5% of the function of two normal kidneys.
So. What does supportive care mean? It means, you will not be discharged, and still be seen regularly – and looked after. The doctors and nurses will focus on dealing with the symptoms described above. There is a lot they (and you) can do. They may also talk to your GP who can get nurses to visit you in your home, and focus on symptom control and holistic (whole person) care.
Some renal units have nurses that specialise in supportive care and symptom control. They may even have their own clinic you can go to. Ask your consultant if your unit has one – if so, ask to be referred.
Summary
We have described the supportive care of CKD. There is a lot that can be done.
Other resources
This is a good paper in a US doctors journal. This is a similar Indian paper.
These are helpful symptom treatment guidelines (and especially good on pain).
Top Tip
Not everyone benefits from dialysis. You may have with a better quality of life, and possibly live longer, without it.
Last Reviewed on 5 April 2024
