Treatment for CKD
Keep track of your kidney data with PKB
In fact, can CKD be treated? Yes, yes and yes.
5 Key Points
- Not all people with CKD need treatment
- Normal (or low) blood pressure – is the single most important thing to do patients with CKD – under 130/80 is ideal
- ‘ACE/ARBs’ and ‘SGLT2 inhibitors’ tablets – can help in many causes of CKD (and diabetes), especially where there is protein in the urine
- Treat some types of chronic glomerulonephritis (with drugs to suppress the immune system), and unblock the kidneys in obstructive nephropathy
- Treat anaemia with erythropoietin (EPO). It is very effective treatment, and will make you feel much less tired.
So. What is the treatment for CKD?
The short answer is yes, CKD can be treated. It cannot usually be cured. But it can often be stabilised and stopped from getting worse. And there is alot both doctors and you can do. Before we describe that, we need to explain some basics first.
Do all people with CKD need treatment?
No. Remember that CKD is a spectrum, ranging from mild damage (CKD1-3A) to advanced disease (CKD4-5) where the kidneys fail to work. Most patients have milder form, and will be able to control their CKD with lifestyle changes, medication regular review, by their GP and practice nurse.
However, 1 in 100 patients with CKD will experience progression of their condition despite these measures, and may ultimately require dialysis or a transplant.
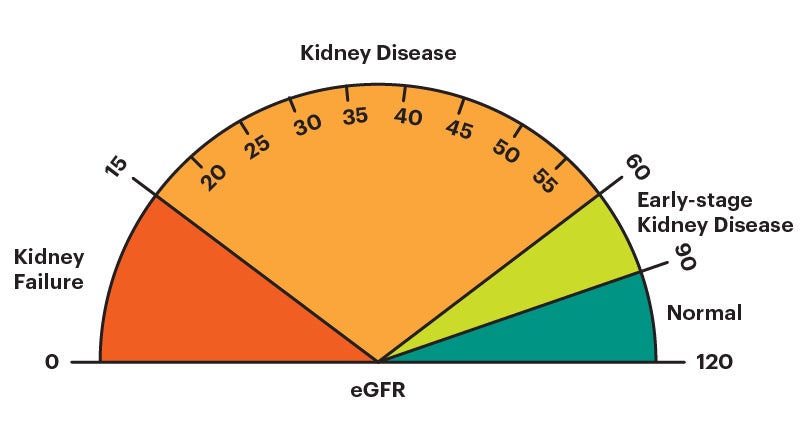
How do doctors decide what to do? They use a classification of severity of CKD (based on something called eGFR) to decide upon whether you need treatment. Normal eGFR in humans is 90-120 mls/min. This divides it up into 5 grades:
- CKD1+2 – risk factors for CKD (eGFR 60-120 mls/min)
- CKD3A+B – mild CKD (eGFR 30-59 mls/min)
- CKD4 – moderate CKD (eGFR 15-29 mls/min)
- CKD5 – severe CKD (kidney failure) (eGFR < 15 mls/min)
Notes
– CKD1, 2 and 3A often need little or no treatment.
– CKD3B is worse than CKD3A.
– CKD4 means you may need dialysis or a kidney transplant one day.
– CKD5 means you require dialysis, or a kidney transplant, or supportive care (no dialysis).
So, what is the objective of treatment for CKD?
This may seem a strange question, as there is no cure for CKD. However, when you are diagnosed with CKD, there are treatments: to help with symptoms; to slow or stop disease progression; and to reduce the risk of heart disease and stroke.
However, despite these measures, 1 in 100 patients will experience progression of their CKD. They may ultimately require dialysis or transplant.
If you need treatment, there are: (1) non-specific CKD treatments (for all causes); and (2) specific CKD treatments (for individual causes). We will now go through the treatment for CKD.
Treatments (general) for all causes of CKD – all grades (CKD1-5)
- Healthy lifestyle. It is a good idea to keep your weight down, exercise, and not to smoke
- Blood pressure (BP) tablets – e.g. Ramipril, Losartan, Bisoprolol, Amlodipine and Doxazosin. The treatment of high BP is more effective if you follow a Low Salt Diet. Talk to your dietitian about that. More on BP treatment on CKDEx here
Having normal (or better low) BP is the single most useful treatment for CKD. Aim for under 130/80 all the time (at home, GP or hospital)
- ACE inhibitors (e.g. Ramipril) and ARB antagonists (e.g. Losartan) – are blood pressure tablets that have a special effect on the kidneys, as they reduce protein levels in the urine, which is damaging. Ask your doctor to be considered for one, if you are not on one
- Sodium-glucose cotransporter 2 (SGLT2) inhibitors (e.g. Dapagliflozin) – are a newish class of drugs that reduce blood glucose levels by increasing urinary glucose excretion. But they have also been shown to be useful for many patients with CKD, especially if there is alot of protein in your urine (with or without diabetes). Again, ask your GP if you are not on one
- Diuretics (‘water tablets’) – e.g. Bendroflumethazide, Furosemide or Bumetanide. Many patients have too much water in the body (shown by ankle swelling and shortness-of-breath). If so, diuretics, which stimulate the kidneys to make more urine, will help
- Control cholesterol – either through dietary means, or HMG-CoA reductase inhibitors (‘statins’).
Note. Yes, this will be a lot of tablets, sorry. But they are necessary, to keep you well. And if they contribute to not getting to the next stage (below), they are worth it.
Treatments (general) for all causes of CKD – higher grades only (CKD4 and CKD5)
- Renal bone disease tablets – e.g. Calcium Acetate and Alfacalcidol (a form of Vitamin D). These are used to increase the calcium, and lower phosphate and parathyroid hormone (PTH) levels in the blood
- Erythropoeitin (EPO). Many patients with CKD4-5 have anaemia (lack of blood in the body) as the kidney makes a substance called EPO that stimulates the bone marrow to make red blood cells. As CKD advances, less EPO is made and anaemia develops.This is easy to treat with an injection once a week (e.g. darbepoetin alfa) or a tablet 3 times a week (e.g. roxadustat) and will give you more energy. Ask your doctor or specialist nurse.When the haemoglobin (‘HB’; marker of anaemia) falls below 100 g/L, EPO should be considered. The target HB is 110-120 g/L. Iron tablets or injections may be necessary too. Ask your doctor or specialist nurse
- Alkali tablets – e.g Sodium Bicarbonate. Some patients have high levels of acid in their blood and these tablets will control that
- Diet. A low protein diet may improve the symptoms of CKD. Talk to your dietitian about that.
NB. Not all patients will need all of these treatments. If they are needed, you need to be seen regularly by a hospital kidney specialist called a nephrologist.
Treatment (non-specific) for all causes (high grade, CKD4 or CKD5) – Preparation for Dialysis and Transplant
- Access referral. ‘Access’ means access to the bloodstream or inside the tummy, to make haemodialysis (HD) or peritoneal dialysis (PD) possible. This can be an operation to create a ‘fistula’ at the wrist or elbow (for HD), or the insertion of a catheter (tube) in the tummy for PD. A fistula should be done at least 3 months from when it is needed
- Transplant referral. Most younger CKD4-5 patients should be referred to start ‘Transplant Work-up’ (tests to check you are suitable, and the best type of kidney for you). Most patients assume that if they are being prepared for dialysis, they are going to be put on the transplant waiting list. Assume nothing. Check check check. You are only on the waiting list when you are written to, and the letter says you are on it
- Living donor? Ask your loved ones to be kidney donor. Again, if you are in the CKD4-5 group, a loved one (partner, friend or relative) may be able to give you a kidney. Ask them. This is best done in a quiet room, one to one, face to face.
Is dialysis or a transplant a treatment for CKD?
No, not really. Dialysis can replace about 5% of the function of two kidneys (about 5 ml/min GFR), and a fully functioning transplant 50% (50-60 ml/min GFR). But they do not treat it, i.e. they do not treat the underlying condition that has caused kidney failure.
Treatments (specific) for individual causes of CKD
CKD is not a diagnosis. It is a syndrome with 7 groups of causes/diagnoses. You need to ascertain the underlying cause as this guides treatment. Here are the different treatments for different causes.
1. Unknown
This is the commonest ’cause’, affecting 30% of people with CKD. It is not really a cause, as the phrase means we do not understand the cause. The kidneys usually become small and scarred over the years. It is presumed to be something you are born with, or a late stage of some of the other causes below.
Specific treatment: There is no specific treatment if the cause of CKD is unknown.
2. Diabetes
Both Type 1 and Type 2 diabetes can affect the kidneys. It is called diabetic nephropathy or diabetic kidney disease. It is the second most common cause, affecting 20% of people with CKD. An increased amount of protein in the urine is characteristic. It usually comes on ten years or more, after the onset of diabetes.
Specific treatments:
- Low blood pressure (BP). It is especially important to make the blood pressure (BP) as low as possible if diabetes is the cause of CKD – under 120/70 all the time (at home, GP or hospital)
- ACE inhibitors (e.g. Ramipril) and ARBs (e.g. Losartan). These are special types of BP tablet that are especially useful if your CKD is caused by diabetes
- Sodium-glucose cotransporter 2 (SGLT2) inhibitors (e.g. Dapagliflozin). This newish treatment for diabetes is especially useful if your CKD is caused by diabetes. Ask your GP or kidney specialist if you are not on one
- Aspirin – should be used for prevention and treatment of heart disease.
3. Renovascular disease (RVD)
This is a common cause in older people, especially if they have smoked. It is also known as renal artery stenosis (RAS = tightening of artery to the kidney). It is due to slow long term furring up (with cholesterol and fat etc) of the main blood vessels (arteries) to the kidneys. It is similar to other diseases that are caused by furring up of blood vessels, e.g. heart attacks, and strokes.
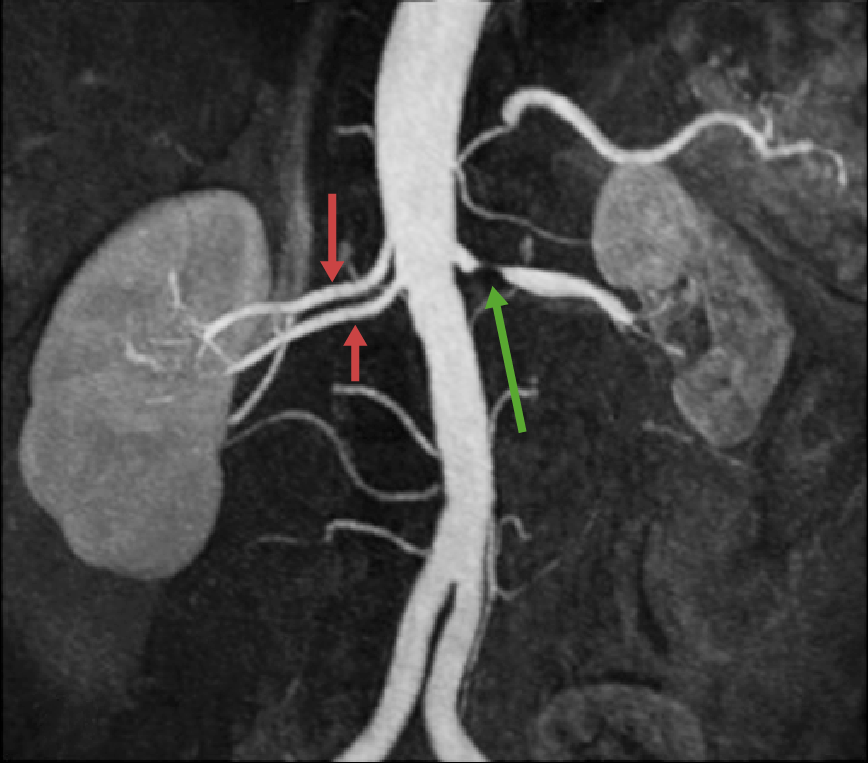
This is a special x-ray called an angiogram that shows a Left renal artery stenosis (green arrow) with two normal renal arteries on the Right. This is a normal variant and quite common (25% of the population)
NB. Some people have more than one cause of CKD. For example, it is quite common for people with diabetes to have diabetic kidney and renovascular disease.
Specific treatments:
- ACE inhibitors/ARBs. These are special BP tablets that can make renovascular disease worse. They may need to be stopped
- X-ray procedure (renal angioplasty +/- stent). A very small number of patients will need a special x-ray treatment when the blockage(s) are squashed, and plastic stent(s) inserted to prevent recurrence of the blockage(s).
4. Chronic glomerulonephritis (‘GN’)
This is an inflammation of the kidney’s filtering units (glomeruli; one million in each kidney). There are 7 subtypes. All are considered an ‘auto-immune’ disease, i.e. something has aggravated the body’s immune (defence) system.
And the immune system is attacking the glomeruli and/or small blood vessels within the kidney. Some of this group are called a ‘vasculitis’. They are similar. For most types, an increased amount of protein in the urine is characteristic.
Specific treatments:
- Low blood pressure (BP). It is especially important to make the blood pressure (BP) as low as possible if GN is the cause of CKD – under 120/70 all the time (at home, GP or hospital)
- ACE inhibitors and ARBs. These are special types of BP tablet that are especially useful in GN
- Sodium-glucose cotransporter 2 (SGLT2) inhibitors (e.g. Dapagliflozin). This newish treatment for diabetes are used if you have alot of protein (like in many people with GN) as part of your CKD. Again, ask your kidney specialist
- Immunosuppression. Some of the 7 types respond to drugs (and other treatments) that suppress the immune (body’s defence) system. These include: Prednisolone; Azathioprine/Mycophenolate; Rituximab; Ciclosporin/Tacrolimus; Cyclophosphamide and Plasma Exchange (a bit like dialysis).
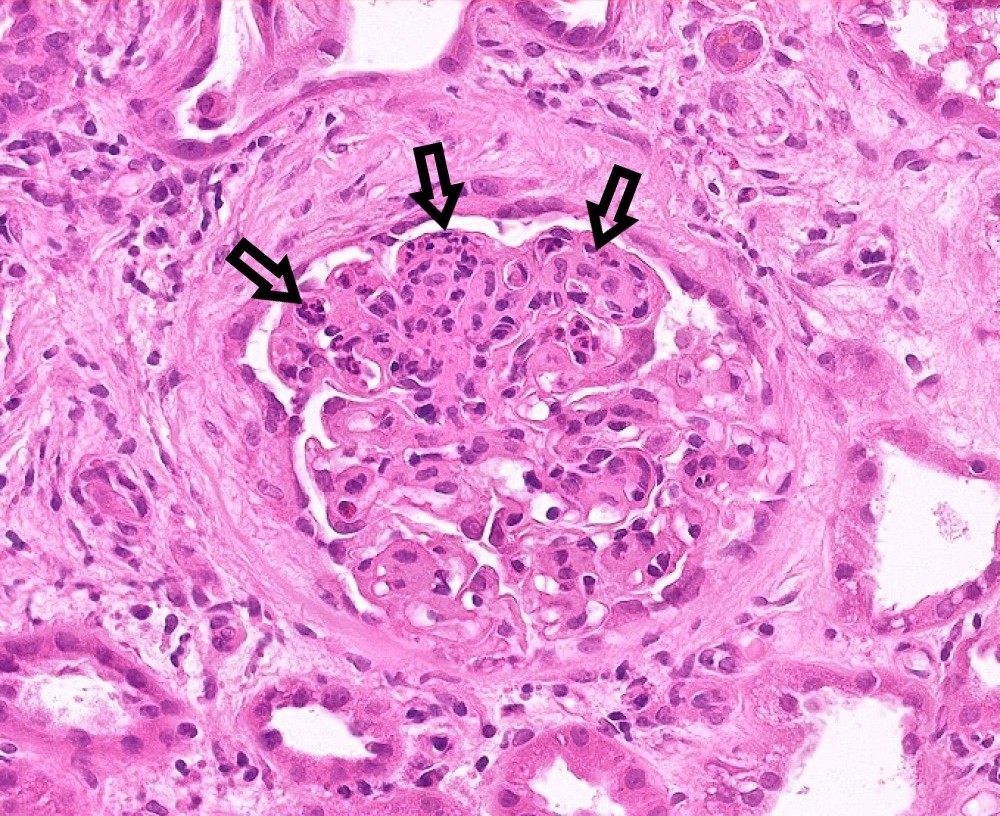
This is a glomerulus (trust us, it is!) one of the million tiny filtering units in each kidney. This one is affected by a type of glomerulonephritis called IgA nephropathy, the commonest type. The arrows point out the affected areas.
5. Polycystic kidney disease (PKD)
This is the only common inherited cause of chronic kidney disease. There are many cysts in both kidneys. It is not really a kidney disease. It can affect the body in many other ways, e.g. cysts in the liver, and other abnormalities in the heart and brain. If you have it, so will 50% of your children.
Specific treatments:
- ACE inhibitors and ARBs. These are special types of BP tablet that are especially helpful in PKD
- Tolvaptan. This is only used for PKD.
6. Obstruction of the urinary tract (kidneys, ureter or bladder)
Both kidneys have to be blocked to cause CKD. Common causes include an enlarged prostate (in a man) and some pelvic cancers (especially in women). Kidney stones rarely block both kidneys. This is the most treatable cause of CKD. So it is very important to make the diagnosis.

Blockage of the left kidney and ureter (tube from the kidney to the bladder). As the other side is not blocked, CKD would not occur
Specific treatment – the kidneys need to be unblocked. This can be done in a variety of ways including the insertion of a catheter (tube) into the bladder; or x-ray or sound treatments (including removing stones) – and operations on the prostate gland (in a man).
7. Chronic tubulointerstitial disease (TID)
This is an inflammation of the kidney’s tubules and surrounding structures. It is a group of diseases with several causes, including:
– Vesicoureteric reflux nephropathy (or ‘reflux’) – is a condition that causes urine to back up into your kidneys, and cause recurrent urine and kidney infections. This affects women more than men, and can be inherited in a complicated way
– Drugs – e.g. aspirin and similar drugs (NSAIDS), and lithium
– Sarcoidosis – and other rare kidney diseases we do not really understand.
Specific treatments (these depend on the cause, and are very different depending on that cause):
- Antibiotics. These are useful for reflux nephropathy
- Stop the drug causing it. If a drug is the cause of TID, then it should be stopped
- Immunosuppression. Prednisolone and other drugs are sometimes used for sarcoidosis and other rare kidney diseases.
If I have CKD, do I need to see a hospital specialist (nephrologist) to be considered for these specific treatments?
For most people the answer is ‘no’. People with milder forms – called CKD1, CKD2 and CKD3A – do not need to be referred. Patients with CKD3B should be discussed with a kidney specialist (called a ‘nephrologist’ or ‘renal physician’).
But. If you have more serious CKD – i.e. CKD4 or CKD5 – your GP should refer you to one of them. You should see a senior doctor, either a consultant (boss), or their deputy called a registrar.
It is important not to be discharged until your CKD is stable. If you are discharged, the hospital specialist needs to give you and your GP a clear monitoring plan, and criteria for referral back. Keep the name of your consultant and his/her secretary’s name, number and email address.
Overview – and how can I help?
Nonetheless, it is important to stay positive about it. If you are seeing a hospital specialist you can really help by keeping good communication going between them and your GP, especially as computer systems don’t always link up.
[“Yeah, thanks, we have spotted that!” Ed]
Summary
We have described treatment for CKD. There is alot doctors and you can do. We hope it has helped you.
[“Wo. That’s complicated.” CKDEx Ed] Yes, it is, sorry.
Top Tip
If your CKD is due to obstructive nephropathy (blocked kidneys) or glomerulonephritis, there are very effective treatments. So it is important your doctors look hard for these with the investigations above – especially the kidney ultrasound and immunology blood tests.
Other resource
Can CKD be cured?
7 treatments for CKD (shorter version)
Single best treatment for CKD
This article was reviewed by Dr Vicki Ayub, Consultant Nephrologist, UHCW Coventry.
Last Reviewed on 23 April 2024
