What are medically unexplained physical symptoms (MUPS)?
These are when a person has physical symptoms that cannot be explained, and no medical cause found. They are very common and affect 1 in 4 people. This is true for people that go to:
Many people have persistent physical complaints, such as dizziness or abdominal or chest pain, that do not appear to be symptoms of a medical condition.
They are sometimes known as ‘medically unexplained physical symptoms’. They can last for many months or years. These symptoms affect daily functioning, interfere with work, and result in over use of healthcare resources. They are more common in women, and people aged 40-50 years but can occur at any age.
MUPS are also estimated to account for approximately 10% of total NHS expenditure for the working-age population.
This doesn’t mean the symptoms are faked or ‘all in the head’ – they are real and can affect your ability to function properly.
One patient said:
I think they must have the sensitivity to realise that if the patient comes to a consultation, if they take the time to come, if they come to open up, it’s because, somehow, that thing is bothering them.
Not understanding the cause can make them even more distressing and difficult to cope with.
Terminology
The term medically unexplained physical symptoms is synonymous to older terms such as:
- Somatic (meaning ‘body’) or psychosomatic illness or disease
- Somatisation or somatoform disorder
- Conversion disorder
- Functional disorder.
The plethora of terms reflects imprecision and uncertainty in their definition, controversy, and care taken to avoid stigmatising affected people.
Common medically unexplained symptoms
These include:
- Pains in the muscles or joints
- Back pain
- Headaches
- Tiredness
- Feeling faint
- Chest pain
- Heart palpitations
- Stomach problems
- Symptoms of UTI but no proven infection the urine.
What is the mechanism of MUPS?
This is unknown. This is a possible mechanism. It has been suggested that people who have anxiety or depression or who focus excessively on their body might be particularly prone to these symptoms.
How can that happen? Anxiety and depression can cause physical symptoms that make depression and anxiety worse, and these can in turn make the physical symptoms worse, creating a vicious circle.
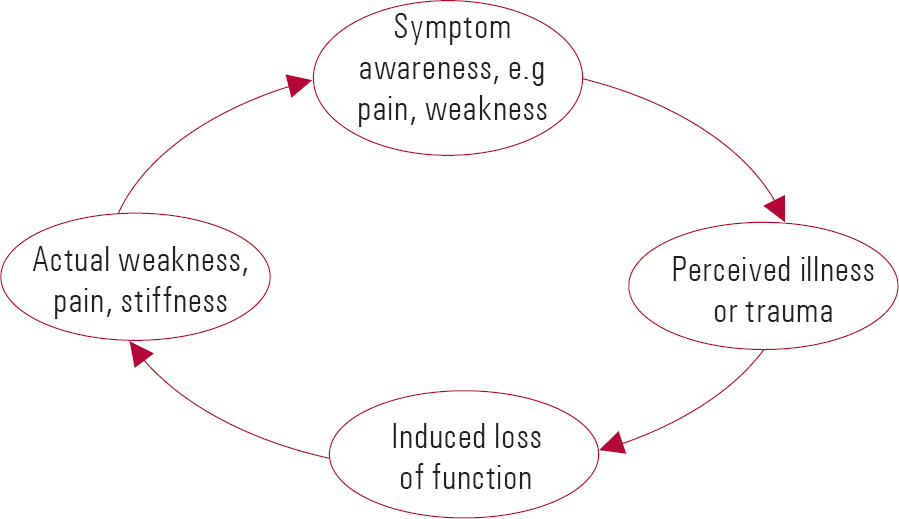 Possible mechanism of MUPS
Possible mechanism of MUPS
Types of medically unexplained symptoms
Many people with medically unexplained symptoms have symptoms such as described above that do not fit into a specific syndrome. Many also have depression or anxiety. Therefore, treating the associated psychological problem can often relieve the physical symptoms.
For others, the symptoms may be part of a poorly understood syndrome, such as:
- Infection
- Chronic fatigue syndrome (CFS) – also known as ‘ME’ (Myalgic encephalomyelitis)
- Long COVID?
- Gastroenterology
- Irritable bowel syndrome (IBS)
- Rheumatology
- Fibromyalgia (pain all over the body)
- Respiratory
- Hyperventilation syndrome
- Renal
- Loin-pain haematuria syndrome
- Urethral syndrome
- Neurology
- Tension headaches
- Non-epileptic attack (pseudoseizure)
- ENT
- Globus hystericus
- Obs and Gynae
- Premenstrual syndrome
- Dentistry
- Temporomandibular disorder (TMD)
- Atypical facial pain
- Unknown
- Food allergy
- Multiple chemical sensitivity
- Gulf war syndrome
- Sick building syndrome.
The fact that doctors are unable to find a cause of symptoms is not unusual in medicine, and it does not mean that nothing can be done to help you.
How a GP can investigate medically unexplained symptoms
A GP will aim to rule out all the medical conditions that might be causing your symptoms. You will need a thorough physical examination, urine and blood tests, and relevant x-rays – to rule out those causes.
The following investigations should be undertaken as a minimum:
- Urinalysis for protein, blood and glucose
- Full blood count
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
- Ferritin, B12 and folate
- Urea and electrolytes – for CKD
- Random blood glucose
- Bone biochemistry
- Liver enzymes
- Thyroid function (TSH)
- PSA (in a man)
- Tissue transglutaminase antibodies (tTG–IgA) for coeliac disease
- Creatine kinase
- Chest x-ray.
Further investigations may be indicated. For example, for persistent unexplained gastrointestinal symptoms in women, particularly for those aged over 50 years, CA125 should be measured.
Common diagnoses which are sometimes missed include diabetes, coeliac disease,Q/M. I wasnt able to do the practical part of assistant coach course on Sunday due to recurrence of back trouble. Will contact IoS and rebook in a couple of months. Will let you know when done. Passed all written exams. Andy thyroid problems and autoimmune conditions.
Second opinion?
However if you doctor is uncertain, and you think you have an underlying condition that has been missed, it is a good idea to ask for a second opinion from another doctor (including referral to the relevant hospital specialist). But after that, repeated specialist referral is rarely useful.
How a GP can manage medical unexplained physical symptoms (MUPS)
Tests (and drug treatment) can be a ritual statement of the doctor’s interest in the patient and their symptoms. But not all patients will want medication. Listening is an important therapy and valued by patients. A ‘caring’ not ‘curing’ approach is best, after an explanation of symptoms.
Another patient said:
Above all, they must know how to listen and give the right amount of advice, without being aggressive or imposing, because these are aspects of a psychological nature and they need to be dealt with very calmly.
The GP should also investigate whether you might have an associated problem, such as depression or anxiety.
It is important to consider whether any medicine you are taking may be causing your symptoms – for example, taking painkillers long term can lead to headaches.
Referral to an IAPT (NHS counsellor) or liaison psychiatrist may help as well.
If your doctors conclusion is that your problems are due to MUPS, it is important that they stop doing tests. Unnecessary CTs for example may find odd things (e,g, a cyst in the liver or kidney, or a small gall stone) that are not a disease, just part of the ageing process. And there are potential iatrogenic risks to further investigation.
Also this article from the Australian Family Physician journal provides useful advice on dealing with patients with MUPS. And this article provides useful advice on the right approach to take.
Things you can do to help yourself
You and the GP may identify some lifestyle changes and goals that you both think will help relieve your symptoms, such as regular physical activity and better rest.
You may be referred for a talking therapy, such as cognitive behavioural therapy (CBT). The aim of CBT is to help you to manage your symptoms by enabling you to understand links between your symptoms, worries, feelings and how you cope.
Medicine such as antidepressants can be helpful, even if you are not depressed.
Self-help
There are things you can do to improve or even relieve some physical symptoms, such as taking regular exercise and managing stress.
Regular exercise will help keep you fit and many people find that it also boosts their mood (read about exercise for depression).
Managing stress is very important because it has been linked to problems such as pain and IBS. Learn about breathing exercises for stress.
Generally, planning some pleasurable personal time to unwind should help – whatever helps you relax, whether it is yoga classes, swimming, running, meditation or walking in the park or countryside.
Outlook
On average 50% of MUPS patients still have MUPS related symptoms, or have developed chronic MUPS, 5 years after diagnosis.
Summary
We have explained what are medically unexplained physical symptoms (MUPS). We hope you understand them better now.
Other resources
Last Reviewed on 20 March 2024
