What are the most common A&E injuries?
Below, in alphabetical order, are 10 common accidents and injuries – many occurring at home – that may need emergency treatment at A&E, and information about how to deal with them:
- Anaphylaxis (or anaphylactic shock)
- Bites (animal and insect)
- Burns and scalds
- Choking
- Drowning
- Electric shock (domestic)
- Head and eye injury
- Falls
- Fractures
- Poisoning (and inhaling toxic fumes).
So. What are the 10 most common A&E injuries?
1. Anaphylaxis
Anaphylaxis (or anaphylactic shock) is a severe allergic reaction that can occur after eating certain foods or an insect sting. The reaction can be very fast, occurring within seconds or minutes of coming into contact with the substance the person is allergic to (allergen).
During anaphylactic shock, it may be difficult for the person to breathe, as their tongue and throat may swell, obstructing their airway.
Phone 999 immediately if you think someone is experiencing anaphylactic shock
What to do – check if the person is carrying any medication. Some people who know they have severe allergies may carry an adrenaline self-injector, which is a type of pre-loaded syringe. You can either help the person administer their medication or, or give it to them yourself.
After the injection, continue to look after the person until medical help arrives. All casualties who have had an intramuscular or subcutaneous (under the skin) injection of adrenaline must be seen and medically checked by a doctor or nurse as soon as possible after the injection has been given.
Top tip for anaphylaxis – make sure they are comfortable and can breathe as best they can while waiting for medical help to arrive. If they are conscious, sitting upright is normally the best position for them.
2. Bites (including animal and insect)
Animal bites (including dog bites)
Most often dog and animal bites are not life-threatening. Often a child is bitten by an animal that he/she is familiar with, although strays are also known to attack in some instances. An animal usually bites when it is provoked or teased; or sometimes if the child is just showing affection and is too close to it.
What to do – immediately wash the area of the bite with soap and water to make sure all the animal’s saliva is washed off. Arrest the bleeding, if any, by applying pressure with a clean cloth or gauze. Then, apply an antiseptic or antibiotic cream on the bite mark, and close it with a sterile gauze or bandage.
It is always advisable for a doctor to check a significant bite to rule out any possible signs of infection. A course of antibiotics may be prescribed. In some cases, a course of injections is required to prevent the spread of rabies.
Monitor your child to check if the wound is deep, skin is broken, the bite area swells, turns red or becomes more painful or if he/she develops a fever. Bites on the face, head, neck or any joint are usually more serious.
Top tip for animal bites – make sure to let the doctor know if the animal was wild, a stray or a pet that has not had its vaccination shots.
Insect bites
Common insect bites include bites and stings from ants, mosquitoes, bees, wasps, certain types of flies and even bed bugs, which can occur indoors or outdoors. These insects feed by biting into the skin to reach into a blood vessel.
While some insects take a quick feed and leave, others can continue to stay on the body until they fall off when they are swollen with blood. Insect bites cause itching as the injected saliva of the insect reacts with the body.
This is usually followed by redness and swelling, and a small raised reddish bump appears on the skin. Sometimes, the skin around the area swells up as well. These symptoms can last from about two hours to even two days.
What to do – you may need to do nothing if the bite is minor. If it is significant, a cold compress or ice can bring down the swelling. Over-the-counter creams from your local pharmacist will also relieve any pain or itchiness. Seek medical help if your child develops a fever, a rash or any other unusual symptoms.
Top tip for insect bites – only use an antihistamine medication when necessary but remember that it causes drowsiness.
3. Burns and scalds
What to do – if someone has a minor burn or scald, you may need to do nothing. If it is significant:
- Cool the burn as quickly as possible with cool running water for at least 10 minutes, or until the pain is relieved
- While cooling the burn, carefully remove any clothing or jewellery, unless it is attached to the skin
- If you are cooling a large burnt area, particularly in babies, children and elderly people, be aware that it may cause hypothermia (it may be necessary to stop cooling the burn to avoid hypothermia)
- Cover the burn loosely with cling film; if cling film isn’t available, use a clean, dry dressing or non-fluffy material; don’t wrap the burn tightly, because swelling may lead to further injury
- Do not apply creams, lotions or sprays to the burn
- Go to A&E (or call 999) without delay, if the burn is really significant.
For chemical burns, wear protective gloves, remove any affected clothing, and rinse the burn with cool running water for at least 20 minutes to wash out the chemical. If possible, determine the cause of the injury.
In certain situations where a chemical is regularly handled, a specific chemical antidote may be available to use.
Top tip for chemical burns – be careful not to contaminate and injure yourself with the chemical, and wear protective clothing if necessary.
4. Choking
The information below is for choking in adults and children over one year old.
Mild choking
If the airway is only partly blocked, the person will usually be able to speak, cry, cough or breathe. In situations like this, a person will usually be able to clear the blockage themselves.
If choking is mild:
- Encourage the person to cough to try to clear the blockage
- Ask them to try to spit out the object if it is in their mouth
- Do not put your fingers in their mouth to help them because they may accidentally bite you
- If coughing doesn’t work, start back blows (see below).
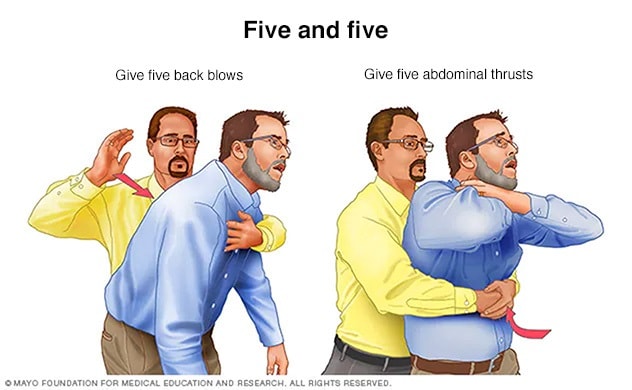
Severe choking – ‘five and five’
If choking is severe, the person will not be able to speak, cry, cough or breathe; and without help they will eventually become unconscious.
To help an adult or child over one year old:
- Stand behind the person and slightly to one side. Support their chest with one hand. Lean the person forward so that the object blocking their airway will come out of their mouth, rather than moving further down
- Give up to five sharp blows between the person’s shoulder blades with the heel of your hand (the heel is between the palm of your hand and your wrist)
- Check if the blockage has cleared
- If not, give up to five abdominal thrusts (see below). Abdominal thrusts should not be used on babies under one year old or pregnant women.
If the obstruction does not clear after three cycles of back blows and chest thrusts, phone 999 to ask for an ambulance, and continue until help arrives.
Top tip for choking – a person with severe choking should be seen by a doctor or nurse afterwards, to check for any injuries or small pieces of the obstruction that remain.
5. Drowning
What to do – if someone is in difficulty in water, only enter the water to help if it is essential. In other words you need to be a good swimmer and don’t think you will get into difficulty.
Once the person is on land, if they are not breathing, open the airway and give five initial rescue breaths before starting CPR. If you are alone, perform CPR for one minute before phoning 999.
If the person is unconscious but still breathing, put them into the recovery position with their head lower than their body and phone an ambulance immediately.
Top for drowning – continue to observe the casualty to ensure they do not stop breathing or airway becomes obstructed.
6. Electric shock (domestic)
What to do – if someone has had an electric shock, switch off the electrical current at the mains to break the contact between the person and the electrical supply.
If you cannot reach the mains supply:
- Do not go near or touch the person until you are sure the electrical supply has been switched off
- Once the power supply has been switched off, and if the person is not breathing
- Phone 999 without delay.
Top tip for electric shock – afterwards, seek medical help – unless the electric shock is very minor.
7. Head and eye injury
Head injury
A head injury can either be external involving the scalp or internal involving the skull and blood vessels within the skull or brain. It is common for children to bump their heads while playing, running or jumping. This can cause a minor bruise, bump or cut on the head. The bump is a result of blood from the veins leaking into and under the scalp. It should disappear in a day or two but sometimes can last longer.
What to do – if it is minor, do nothing. If larger, apply an ice pack on the bump, which will help reduce the swelling and pain. Monitor your child closely.
If he/she has lost consciousness (even for a short time), is dazed, has any abnormality in the way he walks or talks, shows signs of concussion (temporary loss of normal brain function due to injury), starts vomiting or vomits during the one hour after the injury, develops a headache, has blurred vision, memory loss or abnormal breathing, go to A&E (or call 999) without delay. A bleed in the brain may be occurring and need surgery.
Top tip for head injuries – head injuries can be minor or have serious consequences.
Eye injury
Minor eye injuries are common in children with dust, dirt or soap causing irritation to the eye. This results in redness in and around the eye, a burning sensation, watering and mild blurriness in vision. Major injuries include being hit in the eye with a hard object, a chemical entering the eye, or something embedded in the eye that causes bleeding.
What to do – make your child bend over a basin such that her eye faces downwards. Pull down the lower lid gently and pour some lukewarm water over the eye. Repeat this for about two to five minutes. Check to see if the particle, if any, has been dislodged from the eye. If your child has suffered a more serious injury and is in severe pain, go to A&E (or call 999) without delay.
Top tip for eye injuries – keep your child calm. Getting the right treatment in time may prevent blindness. Go to Eye Casualty if needed. Check your local A&E has one before you go; if jot go to a larger regional hospital.
8. Falls
Falls have many causes, from simple trips to life-threatening disease (may be the first sign of). Here are some causes:
- Simple trips (called mechanical falls)
- Low blood pressure (which has many causes)
- Muscle weakness, especially in the legs
- Poor balance, causing unsteadiness on your feet
- Fainting or loss of consciousness
- Foot problems – including pain and deformities
- Memory loss, confusion or difficulties with thinking or problem solving; visual and hearing problems
- Medication that causes low blood pressure or drowsiness
- Alcohol or recreational drug excess or withdrawal.
A fall can affect people of all ages, but it is more common among in young children and older people. Often, when a child falls, it will only take a few words of encouragement to recover.
Top tip for falls – if an older person falls and cannot get up, or is drowsy or confused, take them to A&E (or call 999) without delay.
9. Fractures
It can be difficult to tell if a person has a broken bone or a joint, as opposed to a simple muscular injury. If you are in any doubt, treat the injury as a broken bone.
What to do – prevent any further pain or damage by keeping the fracture as still as possible, until you get them safely to hospital.
Assess the injury and decide whether the best way to get them to hospital is by ambulance or car. For example, if the pain is not too severe, you could transport them to A&E by car.
It is always best (if possible) to get someone else to drive, so that you can deal with the casualty if they deteriorate – for example, if they lose consciousness as a result of the pain or start to vomit.
However, if they are in a lot of pain, do not move them and phone 999. Or if it is obvious they have a broken leg (or back), do not move them; and keep them in the position you found them in and phone 999.
Top tip for fractures – do not give the casualty anything to eat or drink, because they may need a general anaesthetic when they reach hospital.
10. Poisoning
Poisoning is potentially life-threatening. Most cases of poisoning in the UK happen when a person has swallowed a toxic substance, such as bleach, taken an overdose of a prescription medication, or eaten wild plants and fungi. Alcohol poisoning can cause similar symptoms.
If you think someone has swallowed a poisonous substance, go to A&E (or call 999) without delay.
The effects of poisoning depend on the substance swallowed, but can include vomiting, loss of consciousness, pain or a burning sensation.
What to do –
- Find out what has been swallowed, so you can tell the paramedic or doctor
- Do not give the person anything to eat or drink unless
- Do not try to cause vomiting
- If the person becomes unconscious while you are waiting for help to arrive, check for breathing and, if necessary, perform CPR.
Do not leave them if they are semi- or unconscious because they may roll onto their back, which could cause them to vomit. The vomit could then enter their lungs and make them choke.
Top tip for poisoning – if the casualty is conscious and breathing normally, put them into the recovery position and continue to monitor their conscious state and breathing.
Summary
We have described what are the most common A&E injuries or accidents, and what to do if it happens. We hope it has helped you.
Last Reviewed on 24 April 2024
