What is a pelvi-ureteric junction (PUJ) obstruction?
Pelvi-ureteric junction (PUJ) obstruction is a condition where there is a blockage at the point where the renal pelvis (the area where the kidney collects urine) meets the ureter (the tube that carries urine from the kidney to the bladder).
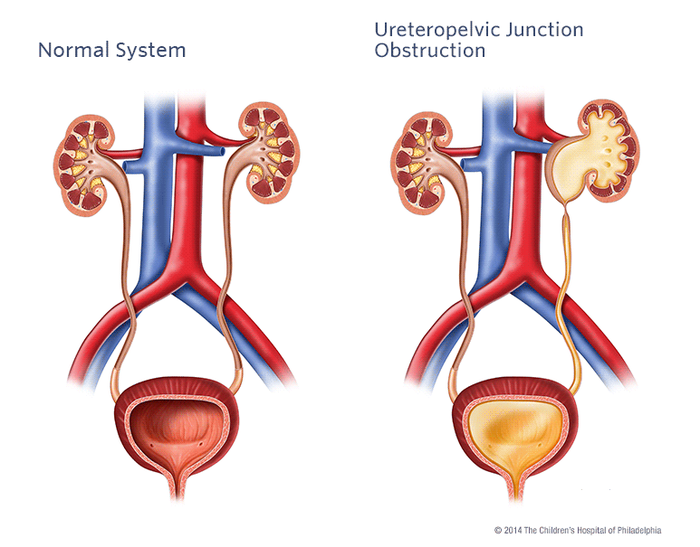
Image provided courtesy of Children’s Hospital of Philadelphia
© The Children’s Hospital of Philadelphia.
Here are 10 key facts about PUJ obstruction.
1. Definition
PUJ obstruction occurs when the drainage of urine from the kidney into the ureter (the tube connecting the kidney to the bladder) is blocked. This leads to swelling of the renal pelvis (hydronephrosis), the part of the kidney where urine drains.
If left untreated, it can lead to kidney damage; and in some severe cases, loss of the affected kidney.
2. Who gets PUJ?
PUJ obstruction can present at any age – from babies to any age of adult. Males are twice as likely to have a PUJ obstruction than females. The left kidney is affected about twice as often as the right.
3. What is PUJ due to?
PUJ obstruction is usually congenital (present from birth) but can be acquired (developed later in life).
If congenital, it results from a developmental abnormality in the structure of the ureter or surrounding tissues.
If acquired, it may result from compression by a blood vessel, or scar tissue due to trauma (or retroperitoneal fibrosis, RPF), infection, or kidney stones.
PUJ obstruction is not hereditary disease – i.e. it is not passed from parents to children.
4. Incidence
Approximately 1 in 750 to 1,000 people will have or develop PUJ obstruction. There are no known risk factors, but it may occur alongside other urinary tract abnormalities.
5. Symptoms
These can vary widely, from none to mild to severe. Some individuals may be asymptomatic; whilst others may experience symptoms such as:
- Abdominal or flank pain – especially after alot of oral fluids, or diuresis
- Recurrent urinary tract infections (UTIs)
- Blood in the urine (haematuria)
- Poor growth in infants (failure to thrive)
- Kidney stones.
6. Diagnosis
Diagnosis of PUJ obstruction often involves imaging studies such as ultrasound, IVP, CT scan, or MRI. These tests help visualise the urinary tract and identify any significant blockage.

IVP showing a right-sided PUJ obstruction
Neonatal diagnosis. PUJ obstruction is the most common cause of neonatally and antenatally diagnosed hydronephrosis. The frequency of unilateral PUJ obstruction is estimated to be 1 case in 5,000 to 8,000 live births.
7. Treatment
In many cases, treatment may not be necessary. However, if treatment is required, success rates are over 90%. Pyeloplasty – a robot-assisted laparoscopic or keyhole operation – is a safe and effective treatment for PUJ obstruction.
8. Complications
The severity of the PUJ obstruction can vary. In some cases, the blockage may only partially impede urine flow; whilst in others, it can completely obstruct the flow of urine from the kidney to the bladder.
In those cases, if left untreated, PUJ obstruction can lead to complications such as kidney damage, hydronephrosis (swelling of the kidney due to urine buildup), or urinary tract infections (UTIs).
9. Prognosis
With appropriate treatment, the prognosis for individuals with PUJ obstruction is good. Most patients experience relief of symptoms and improvement in kidney function after surgery.
10. Follow-up
Follow-up appointments are needed to monitor kidney function, check for recurrence of symptoms, and ensure the success of surgical treatment.
Summary
We have described what is a pelvi-ureteric junction (PUJ) obstruction. We hope it has been helpful.
Other resources
There is more information on PUJ obstruction here on the (very good) childrens kidney website Infokid
Review article: Aaraj, 2023
Last Reviewed on 8 May 2024
