What is an arteriovenous fistula (AVF) for dialysis?
In this article we will describe what is a fistula (or arteriovenous fistula, AVF) for dialysis.
Key points
- An arteriovenous fistula is formed during an operation
- The surgeon joins a vein and an artery together in your arm, in preparation for dialysis
- A fistula enables haemodialysis to take place
- A fistula is a good long-term solution for haemodialysis.
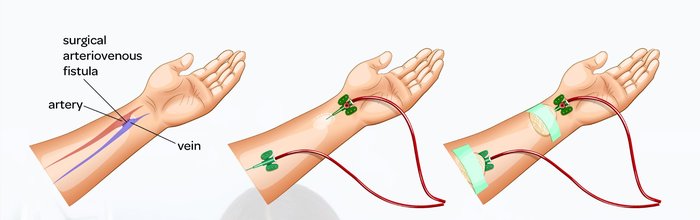
Two needles are inserted into the AV fistula during haemodialysis session – one to remove blood from the body and another to return filtered blood.
Photo. Courtesy of Kidney Care UK
So what is an AV fistula?
A fistula enables haemodialysis to take place. Normal veins used for blood tests are not strong enough for dialysis because blood is pumped through the dialysis machine at high speeds. So we need to create a ‘stronger’ blood vessel.
We do this by connecting a vein to an artery either in the wrist area (radial fistula) or elbow crease (brachial fistula). The operations are done there as there is a pulse below it; which means the artery (taking blood from the heart to the arm and hand) is near the skin.
When this connection is created, fast flowing blood from the artery travels up the vein. The vein adapts to this by gradually thickening up and enlarging and turns into a ‘super-vein’.
At this point the fistula is strong enough to withstand needling on a regular basis and allows for regular haemodialysis.
How is the operation done?
The operation to connect the artery and vein lasts about an hour. It is usually done under local anaesthetic so you are awake. For some fistulas, a general anaesthetic is required.
Once the fistula is created, there will be a ‘buzz’ in the vein. You will be shown how to feel this buzz and it is your way of making sure the fistula is working.
When should a fistula be created?
AVFs should be planned at least 6 months before starting dialysis. This means in Stage 4 CKD when the GFR is 15-29 ml/min and falling (the creatinine will be 300-350 mcmol/L and rising, at this stage). Dialysis is often required in a year at this point.
I.e. they need to be done ‘early’, to give time for a. the fistula to mature (see below); and, b. for a second fistula to be made if the first one does not work.
When can a fistula be used for dialysis?
6-8 weeks after the operation (some take longer). The fistula usually takes 6-8 weeks to ‘mature’; and at this point, it is ready to be ‘needled’ for dialysis.
When first used, the walls of many fistulas are often soft and mobile, and so inserting the needle for the first few haemodialysis sessions may be a little tricky; and bruising can occur at the site of the puncture. This will settle.
Over time, the vessel will become more fixed in position and the vessel wall thickens, and there will be fewer problems when the needle is inserted.

What a ‘mature’ fistula looks like, and being used for haemodialysis
Photo. Courtesy of Kidney Care UK
Maintaining a fistula
Some units check the blood flow in a fistula with a transonic machine or ultrasound every 6 months. Then if a stenosis if forming (see below) it can be dealt with before it becomes a significant problem. However the evidence for doing this is controversial; with some studies showing this practice is useful and others show that it is less useful.
Advantages and disadvantages of an AV fistula
Advantages
- AVFs rarely have infection problems compared to other access methods (e.g. dialysis ‘lines’ or catheters)
- This is because a fistula is internal so does not involve external tubes or artificial material in the body. As the risk of infection is lower, you can swim, have a bath or shower, and take part in water sports with a fistula.
Disadvantages (complications)
- Approximately 30% of fistulas will not work within the first 24 hour, or they will clot off or fail to develop suitably to be used for haemodialysis
- If this happens, you may need a second operation or another procedure to re-establish the flow in the fistula
- If they do work, they usually do not last forever. The average lifespan of a fistula is 3 years (2 years if have diabetes) (Yolgösteren, 2018). Whereas, the average survival of a PD catheter is 18 months (Haught, 2020).
- Aneurysm formation. This means a longterm widening of the fistula. It may lead to the need for ligation (surgical procedure to ‘tie off’ and so stop a fistula)
- Other problems include: thrombosis (clotting), and stenosis (narrowing) of the fistula. A stenosis may need treatment with an xray technique called a ‘fistulaplasty’ (a form of angioplasty).
So many longterm haemodialysis patients will require two or more fistulas. But a ‘good fistula’ can last many years, sometimes decades.
Can everyone have a fistula?
No. Unfortunately, we can’t make a fistula for everyone. There must be a suitably sized vein and artery in the arm. We work this out by examining your arm and ‘mapping’ the arteries and veins with an ultrasound.
In some people, the vein or artery in the arm is not big enough for a fistula. Also, veins in the arms may be damaged by previous blood tests, or by the insertion of IV lines.
All patients with worsening chronic kidney disease (CKD) are advised whenever possible, to protect the blood vessels in their arms ‘Save Your Vein!’. Whenever possible it is best to have blood taken from the back of the hand.
Alternatives to a fistula
There are two alternatives to a fistula:
- Arteriovenous graft (AVG). This is similar to a fistula but uses a plastic tube under the skin to connect the artery to the vein. They are popular in the USA
- Haemodialysis line. This is only really designed to last 3 months or less. If left in, they tend to block or get infected.
Remember that taking care of your access will help your access take care of you.
Summary
We have described what is an arteriovenous fistula (AVF) for dialysis. We hope it has been helpful.
Other resources
What is a fistulaplasty?
Having a fistula or graft (patient information leaflet from UHCW, Coventry)
What is a haemodialysis line?
What is an AV graft?
Review article: Marsh, 2023
Last Reviewed on 14 June 2024
