What is chronic kidney disease of unknown cause?
In this article we will describe what is chronic kidney disease of unknown cause.
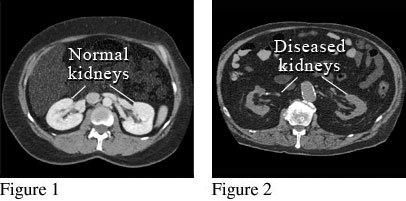
CT of patient (on the right) with CKD of unknown cause and 2 small kidneys. It is impossible to tell the original disease.
1. CKD of unknown cause is common
CKD of unknown cause (also known as ‘idiopathic CKD’) refers to chronic kidney disease where the cause of renal damage is unknown. Despite extensive testing and evaluation, the exact cause remains elusive.
On renal ultrasound (or CT as above) one (or more often both) kidneys are usually small, indicating very long-term damage.
Strangely, it is actually the commonest reason (30%) why patients are in ESRF and on dialysis or have a kidney transplant. Diabetic nephropathy is the second commonest (20%).
2. So what is the ’cause’?
By definition, it is not known. It is assumed that are there are two broad groups:
- Congenital – i.e. born with underdeveloped kidneys (dys/hypoplasia) that start or become small and lose function
- Acquired – a late stage of other (known) causes of CKD, especially renovascular disease, chronic tubulointerstitial disease (TID) or chronic glomerulonephritis (GN) – when the diagnosis may have been missed.
3. Diagnosis
Diagnosis typically involves a combination of medical history and physical examination, urine and tests, and a renal ultrasound (US; or CT if needed).
The ultrasound (or CT) is the key test. It normally shows one or two small kidneys. Or the ultrasound may show normal sized kidneys, often with thin cortices (the outer area of the kidney).
Protein levels in the urine range from normal to high. This may reflect the original disease. For example, high levels of protein may indicate a chronic GN was the primary disease.
A battery of renal (kidney) immunological blood tests are also done. These can help with deciding if a GN was (is) the original disease, and which one. But these tests are not reliable. They can be positive for diseases you don’t have, or negative for ones that you do.
A kidney biopsy is not normally done, for three reasons: (1) technically difficult; (2) increased likelihood of a bleed from the kidney; and, (3) it will usually show long-term scarring (sclerosis) and not the original disease.
4. Variability
The disease’s presentation and progression can vary widely among individuals. For some it may be a mild problem and they may never develop worsening CKD. But some may experience slow deterioration in CKD and end up in ESRF (requiring dialysis or kidney transplant). Whilst others might progress more rapidly.
This variability may be in part due to the: (1) severity of the original disease, and (2) duration of the previous disease process (this may be impossible to know).
5. Geographic clusters
In some regions of the world (outside the UK), clusters of CKD cases have been reported, often in agricultural communities. These are sometimes called ‘CKDu’. This has raised concerns about potential environmental or occupational factors contributing to the disease.
In these clusters, when a biopsy is done, they often show chronic TID. This ‘cluster-type’ of CKDu may be a different disease from the ‘ordinary-type’ we see in the UK. In the ‘cluster-type’ the ultrasound is often normal (hence they can have biopsies) and high blood pressure usually occurs late the disease process.
Some biopsies are done for research reasons, as research doctors are still trying to find the cause(s). Unfortunately this type occurs in countries that do not always have access to good dialysis facilities. This makes research even more important.
One well known cluster is in Central America and is known as Mesoamerican Nephropathy.
6, Environmental factors
Suspected environmental factors linked to CKDu clusters include exposure to air pollutants and hydrocarbons, pesticides, heavy metals, and other toxins commonly encountered in certain agricultural or industrial settings.
7. Heat stress
It is also postulated that heat stress from intense labour, particularly in hot climates, has been proposed as a potential contributor to the development of CKDu.
8. Potential genetic links
Some studies suggest a potential genetic predisposition to both ‘normal’ CKD of unknown cause and CKDu, which could interact with environmental factors in its development.
In one very large study it was shown that patients with CKD (all types including of unknown cause) were 50% more likely to have a relative with it. But it is not clear whether that is a ‘kidney or autoimmune thing’ or just because there is a genetic predisposition to other risk factors for CKD, like diabetes and high blood pressure.
9. Lack of biomarkers
One of the challenges in diagnosing any type of CKD is the absence of specific biomarkers (blood tests) that can definitively identify the condition.
10. Research
Ongoing research aims to identify the underlying causes of both types of CKD of unknown cause; looking for biomarkers, and developing strategies for prevention and management. Raising awareness about the condition is crucial for early detection and intervention.
It’s important to note that research in this area is still evolving, and our understanding of CKD of unknown cause (both types) is constantly evolving as more data becomes available. All such patients should be referred to a hospital kidney specialist (nephrologist). Unless kidney function is only mildly affected, long-term follow-up is recommended.
Summary
We have described what is chronic kidney disease of unknown cause. It is the commonest ’cause’ of ESRF but little is known about it. We hope this has been helpful.
Last Reviewed on 28 June 2024
