What is haemodialysis (HD)?
Keep track of your kidney data with PKB
Key Points
- Haemodialysis (HD) is usually done for 4 hours, three times a week
- Access to the bloodstream is required for haemodialysis, using either a fistula, graft or line
- Haemodialysis can be done at your base hospital, satellite unit (near where you live), or at home
- The main complication is narrowing, blocking or infection in the fistula, graft or line
- You can stay on HD forever.
So. What is about haemodialysis (HD)? Let’s start with the basics.
1. What is dialysis?
Dialysis is a treatment to remove waste products and fluid from your blood. It is needed when chronic kidney disease (CKD) has progressed to a point when your own kidneys can no longer do this. This is called CKD Stage 5, i.e. kidney failure.
Dialysis is one (very important) aspect of your care, but it is only part of your total treatment. There are tablets and injections (like erythropoietin, EPO) that are very important as well.
2. What the two main types of dialysis?
Peritoneal dialysis and haemodialysis are the two main types. Both types provide about 5% kidney function. In this way, they do not ‘cure’ kidney failure, just control it – by replacing some of your kidney function. Most patients start to feel a bit better three months or more after starting dialysis.
When kidneys reach CKD5, they rarely recover. Dialysis is usually permanent (or until you have a transplant).
3. What are the basics of haemodialysis?
In haemodialysis, a machine removes blood from your body, filters it through a dialyser (artificial kidney) and returns the cleaned blood to your body. This is a 3-5 hour treatment, and most patients have it for 4 hours three times a week. Even though the session is usually four hours, the process will take 6-8 hours of your day.
Most patients will also be asked to follow a fluid restriction of 1.5 litres a day, or less. This can be very hard.

Patient connected to haemodialysis machine. Dialyser is within the machine.
4. Does everyone have it for four hours 3x a week?
No. The dose depends on your size. Smaller people may need three hours, 2 times a week; and large people five hours, 4 times a week.
5. Where does haemodialysis happen?
It can take place in:
- Hospital – which has a renal (kidney) unit
- ‘Satellite’ unit – smaller than a hospital unit, and nearer your home
- At home – you can choose to do it at home, including at night whilst you sleep.
For 1 and 2, you will be given some regular ‘slots’ (days/times) to do it – e.g Monday/Wednesday/Friday morning, or Tuesday/Thursday/Saturday afternoon. There are usually three sessions a day, morning, afternoon and evening.
6. What is vascular access?
Before you can start haemodialysis, you will need to undergo a minor surgical procedure to create (vascular) ‘access’ to the bloodstream. This may be a:
- Arteriovenous fistula (AVF; or just ‘fistula’). A surgeon connects an artery and vein in your arm (at the wrist or elbow). They take 6-8 weeks to mature (grow) before they can be used
- Arteriovenous graft (AVG, or just ‘graft’). If the artery and vein are too short to connect, your surgeon will use a graft (soft, hollow plastic tube) to connect the artery and vein. They can be used straight away
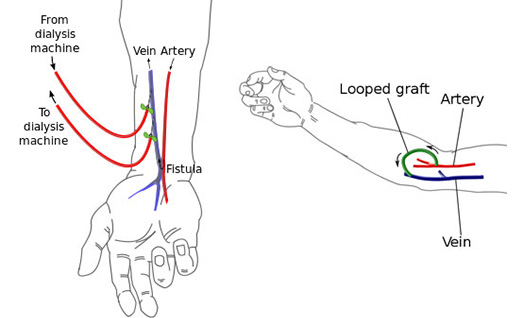 Fistula (left) and Graft (right)
Fistula (left) and Graft (right)
- Central venous catheter (or ‘line’). This is a plastic tube that inserted into the neck vein, with half inside the body, and half outside. It is a temporary measure and should be used for less than 3 months. It is used as temporary access before converting to an AVF (Arteriovenous Fistula) or AVG (Arteriovenous Graft). They can also be used straight away.
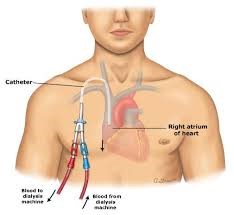
Central venous catheter (‘line’)
With AV fistulas and grafts, the connected artery and vein enlarge, which makes dialysis access easier. When larger, this helps blood flow in and out of your body faster. This is required for good dialysis.
Whichever you have, we call it your ‘access’. And you need to look after it. For example, please do not let anyone take blood or your blood pressure from your fistula or graft arm.
7. What happens during a haemodialysis session?
Before haemodialysis
There is usually a wait of up to 30 minutes as the nurses clean the machine from the previous patient. The wait may be longer if you use hospital transport (see below).
When the nurses are ready, two needles are inserted into the fistula (or graft) and you are attached via tubes to the machine; or if you have a line, the lines two tubes are attached to the machine.
During haemodialysis, the dialysis machine
- Removes blood from a needle in your arm (or tube in the line) , it can also remove any excess fluid if this is an issue for you
- Circulates the blood through the ‘dialyser’ (artificial kidney), which moves waste into dialysis fluid. This cleansing liquid contains water, salt and other additives
- Returns filtered blood to your body through a different needle in your arm (or tube in the line)
- Monitors your blood pressure to adjust how fast blood flows in and out of your body.
 Patient on haemodialysis through a fistula
Patient on haemodialysis through a fistula
The needles are placed in the fistula, with the dialyser just above the middle of this person’s arm
After haemodialysis
Some people experience low blood pressure during or immediately after haemodialysis. This may make you feel nauseous, dizzy or faint.
You will wait about 30 minutes after a session (longer if you use hospital transport, see below), as the nurses need to check you are OK before you go home.
8. What are the complications of haemodialysis?
Problems with fistulas
Narrowing. Fistulas can slowly narrow (forming a ‘stenosis’). There are usually warning signs before blockage, such as difficulty needling, poor flows through the access, or extended post-dialysis bleeding when the needles have been removed.
If this happens the veins should be checked for a narrowing. This will involve an ultrasound scan of your fistula. If there is a narrowing in your fistula this can be treated by having a ‘fistuloplasty’ procedure, in the x-ray department. A fistuloplasty is a procedure where a wire and then balloon are inserted into the fistula to stretch the narrowing in the vein or artery.
Blocking. If a blood clot blocks your fistula completely, you will not be able to feel the ‘buzz’ of the fistula. If this happens, you need to call your renal team urgently, and go to the hospital. A rapid x-ray procedure or operation is needed to remove the blood clot and get the fistula working again. This is more likely to work if you seek help urgently.
Problems with lines
Blockage. Lines can also block. If your line blocks, it may be possible to unblock it with a ‘clot busting’ drug, or to replace it with a new one. The nursing staff can apply these to the line whilst you are present in the dialysis unit.
Infection. Lines can get infected. Keeping a clean dressing over the line reduces the chances of infection. Infection on the line can show itself as either pus (a dirty discharge on the dressing) around the entry point of the line; or blood poisoning with fever and shivers on dialysis. Intravenous (IV) antibiotics will be required. If they do not work, the line will have to be removed.
9. How do you get to/from dialysis (transport)
Patients may drive themselves to have dialysis, or be brought by family or friends. There are usually designated free parking spaces close to the hospital or satellite unit. We would encourage you to travel independently if possible. Why? It is more convenient, and you will not have to spend time waiting for transport.
If you (or family) are not able to bring you up to the hospital (or satellite unit) for dialysis, the renal team will arrange hospital transport for you. Hospital transport drivers need to transport other patients not necessarily from your area, so you will be sharing the transport. Therefore they can take quite a long time to drive to and from the hospital, as several patients will need be picked up and taken home.
10. What are advantages of haemodialysis (and peritoneal dialysis)?
Haemodialysis
Less work for you
Easier to increase dialysis dose
Company of other patients at the dialysis sessions
Easier to get nurses and doctors to see you.
Peritoneal dialysis
Independence
Travelling easier (no travelling required)
Can drink more
As it is continuous, its more like normal kidneys.
Summary
We have described what is haemodialysis (HD). It is not an easy life for a patient, but it is effective and can keep you alive for many years.
Top Tip
If your fistula has stopped (or you think it might do) go to the nearest kidney hospital urgently. You may well need an urgent procedure or operation to get it going, and time is of the essence.
https://www.youtube.com/watch?v=SgBMoCArNak&t=129s
Last Reviewed on 15 May 2024
