What is IgA nephropathy?
IgA nephropathy is one of the 7 types of chronic glomerulonephritis (GN). They are all ‘autoimmune diseases’ where the immune (defence) system attacks normal tissue in the kidney (including the glomerulus). Why and how they occur is unclear.
Who gets IgA?
All GNs are rare. But IgA nephropathy is the most common form of glomerulonephritis worldwide. It can happen at any age, but symptoms most often start before age 40, with a peak onset in the teens and 20s. It is more common in men (70% are male) and in the Far East. It can run in families (<10%).
Causes and types of IgA nephropathy
The exact cause of IgA nephropathy is not fully understood, but it is believed to involve a combination of genetic predisposition and environmental triggers, such as infections leading to a exaggerated autoimmune response. This may be why patients with IgA often get ‘attacks’ of haematuria and loin/back pain after a respiratory or gastrointestinal infection.
IgA is not really a single disease. It has different types, and some types have different causes:
- Primary IgA (most). This type of IgA means that the disease happened on its own without a known or obvious cause. It is presumed to be an autoimmune disease, i.e. caused by your own immune (defence) system attacking the glomeruli within the kidney
- Secondary IgA. This type is caused by another disease:
- Chronic liver disease – particularly alcoholic cirrhosis (thought to be due to impaired IgA immune complex clearance by the liver)
- HIV and AIDS – associated with high blood IgA level
- Coeliac disease – in a small proportion of patients adherence to a gluten free diet can reduce proteinuria and improve kidney function
- Henoch-Schönlein purpura (HSP). IgA nephropathy is closely linked to HSP which is a systemic (whole body) autoimmune disease. In HSP, the IgA antibodies affect not only the kidneys but also other parts of the body, including the skin. A blotchy red rash may appear on the legs and buttocks
- Anti-GBM disease. IgA nephropathy can be the finding on kidney biopsy in anti-GBM disease.

Typical Henoch-Schönlein purpura rash
Symptoms
Some people have no symptoms. But the classic presentation (in 50%) is recurrent macroscopic (visible) haematuria (blood in the urine); or asymptomatic microscopic (non-visible) haematuria with mild proteinuria (protein in urine).
Loin/back/abdominal pain and low-grade fever may accompany acute episodes. Visible haematuria usually begins 1-2 days after an upper respiratory or gastrointestinal illness; thus mimicking postinfectious glomerulonephritis, except the onset of haematuria is earlier (coinciding with or immediately after the febrile illness).
It can also present as chronic kidney disease (CKD, gradual onset kidney failure) or nephrotic syndrome (5%)
In 5% of people, it presents as acute kidney injury (AKI, rarely; rapid onset kidney failure). The kidney biopsy may show a rapidly progressive glomerulonephritis (RPGN). If there are crescents, that can be called ‘crescentic GN’.
Diagnosis
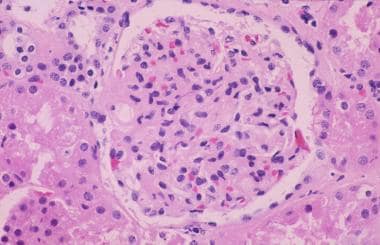
Diagnosis is made through a kidney biopsy, which involves removing a small sample of kidney tissue for examination under a microscope. Biopsy results show the presence of IgA deposits in the glomeruli.
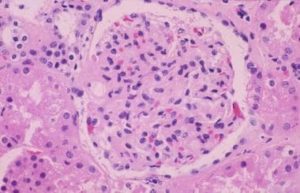
A glomerulus in a patient with IgA nephropathy
IgA levels in the blood are raised in 50% of patients. So even though this test is done, it is not reliable enough to use on its own, i.e. to make (or exclude) a diagnosis of IgA nephropathy.
Treatment
Treatment approaches depend on the severity of the disease. In mild cases, monitoring kidney function and managing blood pressure may be sufficient.
However for many cases, treatment (depending on the type and severity of IgA) may include:
- Medication – such as ACE inhibitors (angiotensin converting enzyme inhibitors) and ARBs (angiotensin receptor blockers) and SGLT2is (sodium-glucose cotransporter 2 inhibitors) to control blood pressure and protein loss
- Fish oil supplements – are sometimes recommended
- Steroids and cyclophosphamide – may be needed for severe AKI due to rapidly progressive glomerulonephritis (RPGN)
- Newer treatments – include budesonide (Barrett, 2023) and sparsentan. There is more about new treatments in other resources below
- Dialysis and/or kidney transplantation. However, IgA nephropathy sometimes recurs in the transplanted kidney (30% at 10 years, Jager et al 2023)
Several new biological agents are being developed for IgA nephropathy at present.
Prognosis (outlook)
Prognosis is very variable. Many individuals experience only minor kidney damage and stable kidney function over time.
But in 25% of patients, within 10 years of diagnosis, chronic kidney disease (CKD) progresses to end-stage renal disease (ESRD; Stage 5 CKD/kidney failure) requiring dialysis or transplantation.
Research
Research into IgA nephropathy is ongoing, focusing on better understanding of its underlying mechanisms, identifying biomarkers for disease progression, and developing targeted therapies (e.g. biological agents) to slow or halt the progression of kidney damage.
History of IgA Nephropathy
IgA is also known as Berger’s disease, and is characterised by a buildup of a type of antibody called immunoglobulin A (IgA) in the glomeruli, the tiny filtering units of the kidneys. IgA is an antibody, that normally protects you from bacteria and viruses. Two French doctors, Jean Berger and Nicole Hinglais, discovered the condition.
Summary
We have described what is IgA nephropathy. Many new drugs for IgA are being introduced at present (including budesonide and sparsentan). We hope it has been helpful.
This article was reviewed by Professor Jonathan Barratt who leads an IgA Nephropathy research team in Leicester. Please contact his team if you would like to take part in a research trial.
Other resources
The IgA nephropathy research team in Leicester has a very good YouTube channel.
New treatments for IgA Nephropathy (Noor, 2023, Caster, 2023)
What is chronic glomerulonephritis?
What is minimal change disease?
What is membranous nephropathy?
What is FSGS?
What is post-infectious glomerulonephritis?
What is mesangiocapillary glomerulonephritis?
What is rapidly progressive glomerulonephritis?
There is more information on IgA nephropathy written by the renal team from UHCW, Coventry.
Last Reviewed on 24 May 2024