What is membranous nephropathy (MN)?
Membranous nephropathy (MN) is one of the 7 types of chronic glomerulonephritis (GN). They are all ‘autoimmune diseases’ where the immune (defence) system attacks normal tissue in the kidney (including the glomerulus). Why and how they occur is unclear.
MN is called membranous nephropathy as immune complexes (antigen-antibody combination) are deposited on the glomerular basement membrane (GBM) causing GBM thickening.
MN mainly affects adults, though can occur at any age. It is the second commonest cause of nephrotic syndrome in adults after FSGS. It most commonly occurs above 40 years of age, with the peak incidence between 50 to 60 years.
MN can be broadly classified into primary (no known cause) or secondary (with a range of causes, see below).
What causes membranous nephropathy?
MN is not caused by a single disease. It has different types, and many different causes:
- Primary MN (80%). This type of MN means that the disease happened on its own without a known or obvious cause. It is presumed to be an autoimmune disease, i.e. caused by your own immune (defence) system attacking the glomeruli within the kidney
- Secondary MN (20%). This type is caused by another disease or a drug. Examples include:
- Infections (hepatitis B and C, syphilis, malaria, HIV, schistosomiasis)
- Cancers (lung, breast and gastrointestinal tract; and some haematological malignancies, like Hodgkin or non-Hodgkin lymphoma). MN may precede the cancer in 40%, and by up to 12-18 months
- Drugs (non-steroidal anti-inflammatory drugs, anti-tumour necrosis factor-alpha inhibitors, penicillamine, probenecid)
- Heavy metals (gold, mercury)
- Other autoimmune diseases (systemic lupus erythematosus (SLE), Sjogren syndrome, rheumatoid arthritis, IgG4 related nephropathy).
Symptoms
The most common presentation of MN is nephrotic syndrome, which shows itself as ankle/leg/peri-orbital oedema (swelling), fatigue, and appetite loss. High blood pressure is another common feature.
Chronic kidney disease (CKD) can develop (usually quite slowly) in some patients. Some of these patients go to develop CKD5 (kidney failure) and need dialysis, and/or a kidney transplant (but MN can sometimes come back in the new kidney).
Diagnosis
Diagnosis of MN is made through medical assessment by a kidney specialist (nephrologist), blood and urine tests, and a kidney biopsy. High cholesterol levels are common as well. Antibodies against phospholipase A2 receptor (PLA2R) antigen are common in cases of primary MN. PLA2R antibodies were discovered in 2009.
Microscopic (i.e. that you cannot see) haematuria (blood in the urine) is present in 50% of people with MN.
A CXR should be done for a possible underlying lung cancer. Other blood tests and scans may be necessary to exclude other secondary causes.
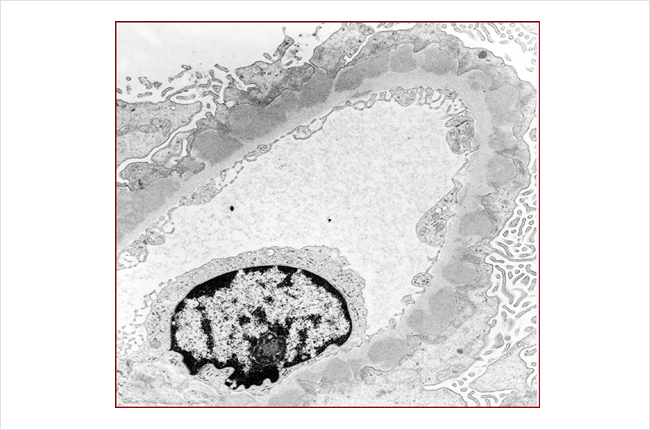
Typical renal biopsy on electron microscopy in MN. The immune deposits are the circular lumps within the outer layer of the glomerular basement membrane (GBM) of the glomerulus
Treatment
Treatments (depending on the type and severity of MN) may include:
- Medicines – such as ACE inhibitors (angiotensin converting enzyme inhibitors) and ARBs (angiotensin receptor blockers) and SGLT2is (sodium-glucose cotransporter 2 inhibitors) to control blood pressure and protein loss
- Steroids – to treat nephrotic syndrome and diuretics (water tablets) to reduce oedema
- Other immunosuppressants (drugs that dampen down the immune system) – may be needed. These include cyclophosphamide, chlorambucil, tacrolimus and ciclosporin, mycophenolate and rituximab
- Cholesterol lowering drugs – may be necessary
- Blood thinning drugs – may be needed to prevent blood clots
- Dialysis and/or kidney transplantation. Membranous nephropathy recurs in about 10% of patients, with loss of the kidney in up to 50%.
For secondary causes, it is important to treat (and remove, if possible) the underlying cause – e.g. remove the cancer.
Prognosis (outlook)
Up to a third of patients diagnosed with MN will go into remission (it will go away) spontaneously within 5 years, even without immunosuppressive therapy. Complete recovery is the rule in MN, if the offending cause is dealt with (e.g. drug is stopped or infection treated).
Over the longer term (decades) about 1/3 of patients will progress to end-stage kidney disease (CKD5 or kidney failure, needing dialysis), about 1/3 will have continued protein in the urine without kidney failure, and about 1/3 will be in remission (disease has gone away).
Of the patients that progress to ESRD, 30% are dead or on dialysis at 5 years, 70% at 10 years, and 80% at 15 years.
However, relapse is common in MN, and patients that go into remission either spontaneously or in response to immunosuppressive medication, can have the disease return later.
Summary
We have described what is membranous nephropathy (MN). We hope you have found it helpful.
Other resources
This is a good review article (for health professionals): Ronco et al, 2021
What is chronic glomerulonephritis?
What is minimal change disease?
What is FSGS?
What is IgA nephropathy?
What is post-infectious glomerulonephritis?
What is mesangiocapillary glomerulonephritis?
What is rapidly progressive glomerulonephritis?
https://www.youtube.com/watch?app=desktop&v=eXAj2PhFRuQ
Last Reviewed on 31 May 2024
