What is minimal change disease (MCD)?
Minimal change disease is one of the 7 types of chronic glomerulonephritis (GN). They are all ‘autoimmune diseases’, where the immune (defence) system attacks normal tissue in the kidney (including the glomerulus). Why and how they occur is unclear.
MCD is the most common cause of nephrotic syndrome in children, accounting for about 85% of cases. MCD typically occurs in children between the ages of 2 and 6, although it can affect people of all ages. It accounts for 10-20% of (primary) nephrotic syndrome in adults.
The name ‘minimal change disease’ comes from the fact that the kidney tissue appears nearly normal under a microscope; and the damage is only visible with an electron microscope (which gives a more detailed picture than a normal (light) microscope).
Fortunately, chronic kidney disease (CKD) does not normally occur, and kidney failure (CKD5) is very rare.
Cause
The exact cause of MCD is unknown, but it is believed to be a autoimmune disease – i.e. your immune (defence) systems is attacking the glomeruli in the kidneys.
MCD is not caused by a single disease. It has different types, and different causes:
- Primary – most MCD cases are ‘primary’ (idiopathic), which means the exact cause is not known
- Secondary – a few people have secondary causes for MCD, and the disease may occur with (or be related to): allergic reactions; non-steroidal anti-inflammatory drugs (NSAIDs) and rarely some other drugs; some cancers (including bone marrow cancers like Hodgkin’s lymphoma and leukaemias) and infections.
Symptoms
Common symptoms of MCD include those of nephrotic syndrome, i.e. swelling (oedema), especially around the eyes and in the ankles and feet, foamy urine due to excess protein loss, and fatigue.
The onset of symptoms is usually quite rapid, more rapid than other causes of nephrotic syndrome (e.g. diabetes or other types of chronic glomerulonephritis) – and in 2/3rds, it may follow an upper respiratory tract infection (URTI).
Diagnosis
Diagnosis is made through a medical assessment by a kidney specialist (nephrologist), blood and urine tests, and a kidney biopsy (in adults) – analysed by electron microscope – to confirm the characteristic changes.
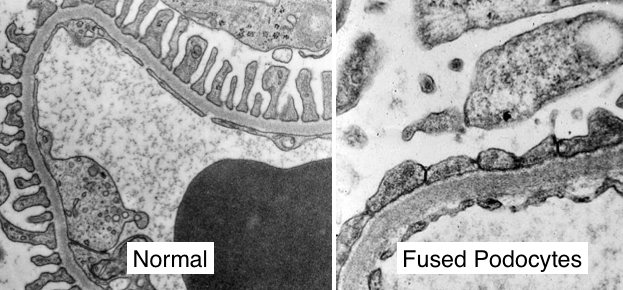
This is an electron microscope picture of the glomerular basement membrane (GBM) of a glomerulus in a kidney biopsy in MCD, with a comparison to a normal one. The (normal) light microscope picture (not shown) is characteristically normal.
Treatment
MCD is usually treated with a steroid medication like prednisolone. In most cases, this treatment leads to a complete remission of the disease. Other medicines are also usually needed:
- ACE inhibitors (angiotensin converting enzyme inhibitors) and ARBs (angiotensin receptor blockers) and SGLT2is (sodium-glucose cotransporter 2 inhibitors) – to control blood pressure and protein loss
- Diuretics (water tablets) – to reduce oedema
- Cholesterol lowering drugs – may be necessary
- Blood thinning drugs – may be needed to prevent blood clots.
90% respond to this initial treatment with prednisolone and other drugs. They can all be stopped when the MCD is successfully treated and the disease has gone away.
When in remission (i.e. its ‘gone away’) patients should be given a urinary dipstick kit; so they can test their own urine for protein in they think the disease has come back, as shown by ankle swelling and/or frothy urine. They should then restart prednisolone soon.
MCD treatment in children
Because MCD is the most common cause of nephrotic syndrome in children, they first get treated for MCD before getting a biopsy. Most people will have a response in fewer than 8 weeks. If the protein in the urine disappears, the doctors may call the disease ‘steroid-sensitive nephrotic syndrome’ instead of MCD.
If treatment does not improve their symptoms over the course of several months, a biopsy is done to see if there is another cause for their symptoms. This is because MCD almost always responds to steroids.
Relapse
Relapse is quite common, occurring in 40-50% of patients in the first six months, after discontinuing steroid treatment – but these relapses often respond well to the same medication.
Some patients relapse frequently, developing ‘steroid-resistant MCD’ and require stronger drugs like ciclosporin (or cyclophosphamide, chlorambucil or mycophenolate) to keep it under control.
Patients that have not relapsed by five years, are typically ‘cured’. Such patients can be discharged.
Prognosis (outlook)
In the majority of cases, MCD has an excellent prognosis. With appropriate treatment, most patients achieve remission and lead a normal life. However, there may be occasional relapses.
Kidney failure (CKD5) and the need for dialysis and/or a kidney transplant, is rare. In fact, it is thought that if you do, the diagnosis is wrong and you actually have another more serious GN like focal segmental glomerulosclerosis (FSGS). Though there may also be an overlap between these two forms of GN, i.e. they may be part of a spectrum, and MCD can transform into FSGS.
This can happen if the doctor accidentally biopsies a normal part of the kidney in FSGS. This happens partly as the biopsy taken is very small.
Complications
MCD itself does not typically lead to severe kidney damage. But the long-term use of steroids – especially if you have frequent relapses – can cause side effects and complications, including osteoporosis, weight gain, and susceptibility to infection.
Summary
We have described minimal change disease. We hope it has been useful.
Other resources
This is a good review article (for health professionals): Zamora, 2023
What is chronic glomerulonephritis?
What is membranous nephropathy?
What is FSGS?
What is IgA nephropathy?
What is post-infectious glomerulonephritis?
What is mesangiocapillary glomerulonephritis?
What is rapidly progressive glomerulonephritis?
Last Reviewed on 25 June 2024
