What is polycystic kidney disease (PKD)?
Polycystic kidney disease (PKD) is a genetic disorder that affects both kidneys from birth, leading to the growth of multiple cysts within the kidneys.
So. What is PKD? Here are 10 facts about the most commonest genetic kidney disease.
1. How rare is PKD?
ADPKD occurs in all races, and is quite common, occurring in approximately 1 in every 400-1000 live births. It is the underlying cause of kidney disease in approximately 10 percent of dialysis patients, and is the commonest inherited cause of CKD and ESRF.
2. What causes CKD (genetic basis)?
PKD is an inherited disorder, caused by mutations in specific genes. The two main types are autosomal dominant PKD (ADPKD) and autosomal recessive PKD (ARPKD) – with ADPKD being the more common form.
3. Types of PKD
Autosomal dominant PKD (ADPKD)
ADPKD is predominantly caused by mutations in one of two genes: ‘PKD1’ on chromosome 16 (80%) and ‘PKD2’ on chromosome 4 (15%). In 5% the genetic abnormality is unknown.
Patients with PKD2 have a less severe disease than those with PKD1, but neither disorder is benign. One parent with the faulty gene has a 50% chance of passing the condition to their children.
The diagnosis is usually made in people when they are in their 20s and 30s using a renal (kidney) ultrasound
Amongst most patients, kidney function remains normal until the patient is in their late 30s/early 40s, then kidney function declines slowly over time.
About 50% go on to develop end-stage renal failure (ESRF) by the age of 60 years; and will need dialysis or kidney transplantation. The average age of the onset of ESRF is 55 and 75 years for PKD1 and PKD2.
Autosomal recessive PKD (ARPKD)
ARPKD is caused by mutations in the PKHD1 gene. It is a more severe form that presents earlier in life, often in infancy or childhood. Both parents must carry a copy of the faulty gene for a child to have ARPKD.
It is a severe disease usually linked to pulmonary hypoplasia (poorly developed lungs) that leads to respiratory (lung) failure and death in ∼30% of affected newborns. If the baby survives, it is an important cause of chronic kidney disease (CKD) and ESRF in children.
4. Cyst formation
In PKD, 1000s of fluid-filled cysts develop in the kidneys. Over time, these cysts grow in size and number, causing the kidneys to enlarge and potentially impair their function. It is also linked to medullary sponge kidney.
The kidneys in PKD can become very big
5. Symptoms
Common symptoms of PKD include: pain or discomfort in the abdomen, sides, or lower back; high blood pressure, frequent urinary tract infections, kidney stones, and blood in the urine.
Or there may be no symptoms and its picked up when investigating (especially a younger person) with high blood pressure (hypertension); or sometimes at a routine medical.
Alternatively, the patient may know they have a family history of relatives on dialysis and/or with a transplant – so go looking for it at a younger age. It’s best to wait until you at least 18 years before you have an ultrasound (the key test for PKD).
6. PKD and CKD (kidney function)
As the cysts grow, they can replace healthy kidney tissue, leading to a decline in kidney function. This can result in chronic kidney disease (CKD), and eventually end-stage renal failure (ESRF) – when dialysis or a kidney transplant will be required.
7. Diagnosis
Imaging tests such as ultrasound, CT and MRI, are used to diagnose PKD, by visualising the cysts in the kidneys. Genetic blood testing has a limited role, as a ‘negative’ test does not mean you do not have it. But it can help confirm the specific type of PKD in some patients.

Typical appearance of PKD on a kidney ultrasound. There are usually cysts in other organs including the liver and spleen.
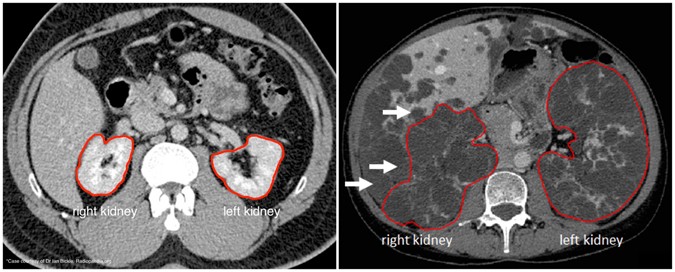
CT scan. Normal scan on left. PKD in both kidneys on right (note cysts in liver as well)
8. Treatment
Whilst there is no cure for PKD, treatment focuses on managing symptoms and slowing disease progression. Tight blood pressure control is crucial to protect kidney function. Pain management strategies and dietary changes (sodium restriction) might also be recommended.
Blood pressure tablets called angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs) are especially effective in PKD. And a tablet called Tolvaptan (a selective vasopressin V2-receptor antagonist) should also be considered.
Despite all interventions, a number of patients will go on to need dialysis (+/- a kidney transplant). In PKD, kidney function deteriorates slowly.
So there is often time to organise a kidney transplant from a living relative (or friend) before dialysis. This is the best option for younger people with PKD approaching or on dialysis due to the disease.
9. Effects of PKD outside the kidneys
Interestingly, PKD is not actually a kidney disease. It is actually a ‘systemic’ (whole body) disorder with cysts and connective tissue abnormalities involving many organs. But it primarily shows itself in the kidneys.
So, it can also affect organs outside the kidneys. For example, there may be cysts in the liver, spleen, ovaries (and elsewhere), particularly in those with ADPKD.
Heart valve abnormalities and aneurysms in the brain’s blood vessels are also associated with PKD. For this reason it is important to examine the patient thoroughly, especially the heart.
10. Research
Ongoing research is exploring potential treatments that could slow or halt the growth of cysts and improve kidney function in PKD patients. Clinical trials and genetic studies are contributing to a better understanding of the disease, and potential therapeutic avenues.
Summary
We have described what is polycystic kidney disease (PKD). We hope it has been helpful.
Last Reviewed on 23 January 2025
