What is chronic tubulointerstitial disease (TID)?
Chronic tubulointerstitial disease is not really one diagnosis. It is not a single disease. The phrase refers to a group of kidney disorders that primarily affect the ‘tubules’. These are the structures largely in the inner area of the kidney (medulla) responsible for processing urine after it has been filtered by the glomeruli. The tubules are shown in the diagram below. Each glomerulus has a tubule and together they are called a ‘nephron’.
The phrase chronic tubulointerstitial disease has largely replaced the older phrase ‘chronic pyelonephritis’ (CP).
Diagram of urinary tract, glomeruli and tubules
Whatever the cause, TID is a very variable disease, sometimes causing a few problems, sometimes only affecting one kidney and total kidney function is normal; and sometimes causing kidney failure (CKD5, requiring dialysis and/or a renal (kidney) transplant. Occasionally the removal of one kidney (nephrectomy) is necessary.
The challenging aspect of chronic TID is the nonspecific and highly variable clinical presentation. This can delay the diagnosis and treatment, worsening the outcome.
Here are 10 facts about chronic tubulointerstitial disease.
1. Definition
Chronic tubulointerstitial disease (TID; also known as chronic tubulointerstitial nephritis, TIN) is a progressive condition characterised by inflammation and scarring of the tubules and interstitium within the kidneys.
2. Causes
Chronic tubulointerstitial disease has three main groups of causes:
- It can be caused by recurrent UTIs due to reflux nephropathy, in which the kidneys are damaged by the backward flow of urine into the kidney – due to a leaky valve between the bladder and the ureter

- Prolonged exposure to certain medications (e.g. beta-lactam antibiotics, sulphonamides, proton pump inhibitors (PPIs), 5-aminosalicylates, rifampicin, lithium and NSAIDs) and toxins (heavy metals). In some patients, when NSAIDs are the cause, the chronic TID is called ‘analgesic nephropathy‘
- Autoimmune disease (e.g. SLE, sarcoidosis). These may respond to suppressing the immune system.
In a few patients, no cause is found, or there are genetic factors. Other causes include myeloma (that an affect the glomeruli (filtering units) as well). In a rare type is called ‘tubulointerstitial nephritis with uveitis (TINU)’ syndrome. Uveitis is an autoimmune eye disease.
3. Symptoms
In some patients the disease is very mild and there are no symptoms.
Characteristically, in many patients, in the early stages of the disease, oedema is not usually present, and blood pressure is normal or only mildly elevated. In others, symptoms include recurrent UTIs, loin/back/abdominal pain; and, if chronic kidney disease (CKD) develops, there may be swelling in the legs and ankles (oedema) and high blood pressure.
4. Kidney function impairment
As the disease progresses, the kidneys’ ability to filter waste products, regulate electrolytes (salts), and maintain fluid balance becomes impaired, leading to kidney dysfunction.
5. Diagnosis
Blood creatinine may be raised (and eGFR low) if it has led to chronic kidney disease (CKD). Urine tests may show infection and normal or low-to-moderate levels of protein. Other tests include:
- Kidney ultrasound or IVP (intravenous pyelogram – a special x-ray) showing scarring, or a small kidney or kidneys. The ultrasound is done partly to check there are two kidneys (as a renal biopsy may be necessary in a few cases) and partly to exclude other diagnoses
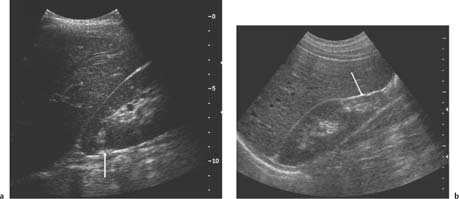 Renal ultrasound
Renal ultrasound
a – A small scar at the upper pole of the right kidney (arrow); b – More marked scarring at the lower pole of another right kidney (arrow). These changes are consistent with chronic TID due to reflux nephropathy (and other diagnoses).
- Nuclear medicine scan
- Computed tomography (CT)
- Micturating cystourethrogram (MCU) – for ?reflux nephropathy. This will usually not be necessary.
A renal biopsy is not usually done, but may be necessary especially if a medication or autoimmune cause is suspected.

A typical renal biopsy in chronic TID. A biopsy is not always necessary.
6. Scarring and fibrosis
In chronic tubulointerstitial disease, ongoing inflammation and injury can lead to the formation of scar tissue (fibrosis) within the kidney. This can gradually replace healthy tissue, impair kidney function and leads to chronic kidney diseases (CKD).
7. Treatment
Simple, uncomplicated CP may require no treatment. When it is needed, treatment aims to manage the underlying cause of the disease, if identified. This involves discontinuing nephrotoxic medications, treating infections, managing autoimmune conditions, and controlling blood pressure.
Specific treatments may be needed depending on the cause:
- Reflux nephropathy – long-term antibiotics. Rarely patients with reflux require surgery to place the ureter(s) back into the bladder to stop the refluxing of urine. If a kidney is thought to be the source of more of the UTIs, and is causing problems (e.g. pain), it should be removed (nephrectomy) – so long as x-ray tests show that it is not making effective urine
- Medication – stop causative medication
- Autoimmune – corticosteroids (e.g. prednisolone).
Even though there is no specific treatment for most patients with CP, keeping the BP low (<130/80) may slow the progression to CKD.
Blood pressure tablets like angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) may slow disease progression – so should be favoured. SGLTis (e.g. Dapagliflozin) should be added to an ACE/ARB, if the patient is proteinuric (protein in urine).
In some cases, dialysis or kidney transplantation might be necessary if kidney function declines significantly.
8. Acute tubulointerstitial disease (TID)
This is a different disease but usually has a drug cause; so overlaps with one group of causes of chronic TID. It usually presents as Acute Kidney Injury (AKI; rapid onset kidney failure).
The classical presentation of a drug-induced hypersensitivity also comprises a triad of symptoms: fever, rash and eosinophilia (raised eosinophil white cells in the blood) – related to the recent use of a new drug (especially antibiotics and PPIs). Though all three features of the classic triad (fever, rash, and eosinophilia) are found in only 10% of cases.
The disease has a good outlook, and usually resolves when the causative drug is stopped. And a short course of corticosteroids (e.g. prednisolone) is usually used.
9. Prognosis
The outlook of chronic TID is very variable. Many patients have little problem, just the occasional kidney infection. Others require regular monitoring by a hospital kidney specialist (nephrologist). Some patients will, however, require long-term dialysis or a kidney transplant.
The prognosis depends on the underlying cause, the extent of kidney damage, and how early the disease is diagnosed and treated. Early intervention can slow the progression of the disease and help preserve kidney function.
10. Prevention
To reduce the risk of developing chronic tubulointerstitial disease, it’s important to avoid prolonged use of nephrotoxic medications, and seek medical attention promptly if you experience symptoms that might indicate kidney problems.
Remember that problems linked to chronic tubulointerstitial disease are very variable, based on the underlying cause and individual patient characteristics. So it is essential to see a hospital kidney specialist (nephrologist) to have guidance tailored to your condition.
Summary
We have described what is chronic tubulointerstitial disease (TID). We hope it has been helpful.
Last Reviewed on 30 April 2024
